There is no one right answer to the question of which imaging test is best for patients with hearing loss who are candidates for cochlear implantation (CI). Age, underlying pathology and the ability to tolerate radiation and sedation are just a few of the variables that can determine whether magnetic resonance imaging (MRI), computed tomography (CT) or both are chosen in this clinical setting.
Explore This Issue
May 2012At least, that’s the current state of affairs in pre-operative CI staging. Twenty years ago, the choice was far simpler, according to Blake C. Papsin, MD, director of the Cochlear Implant Program at the Hospital for Sick Children in Toronto, Canada. “CT scan was the go-to diagnostic tool,” Dr. Papsin said. “It gave us a very detailed picture of the bony structures of the inner ear, and it helped us diagnose the likely cause of the hearing loss, albeit with some radiation exposure. Basically, it gave us a roadmap for how to proceed with CI implantation or other interventions.”
But all of that changed in the mid-2000s, Dr. Papsin noted, when MRI technology had advanced to the point where its advantages, primarily the lack of any radiation exposure and the ability to yield much better images of soft tissue, resulted in serious consideration of the newer imaging test.
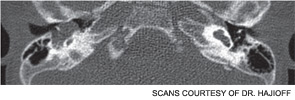
To nail down the relative strengths of each scan, Dr. Papsin and colleagues conducted a head-to-head trial of both imaging modalities and published the results in 2007 (Otol Neurotol. 28(3):317-324). In the prospective study, 92 pediatric patients with hearing loss underwent pre-operative imaging of the petrous temporal bone using both CT and MRI. The study showed that each scan did have some shortcomings. In the case of CT, for example, the test failed to consistently detect early obliterative labrynthitis and the presence of the cochlear nerve in the internal auditory canal. The MRI test often missed the presence of enlarged vestibular aqueducts and narrow cochlear nerve canals. The study’s conclusion that “dual-modality imaging,” using both CT and MRI, made sense for many patients because the dual-scan approach “detects abnormalities related to deafness that would not otherwise be found using either modality alone.”
But do the respective abnormalities missed by each scan truly impact the surgical approach in CI patients? In Dr. Papsin’s experience, not always. In fact, during the study, he and his colleagues initially only looked at the MRI results to see if they would yield enough diagnostic information to guide their hands during surgery. “We agreed, based on the design of the study, that if those MRI scans sufficed, we would not ‘break the code’ and ask to see the CT results,” he said. “Well, we never broke the code during the study. Yes, the MRIs missed some things, as the findings pointed out. But those diagnostic ‘misses’ were not enough to change how we treated the patients.”
Thus, for some patients, typically adults or teens, Dr. Papsin is currently satisfied with obtaining only an MRI. “It gives me all the information I need, and if I do see a structural abnormality that gives me pause, I can bring these patients back at another time for a CT scan; they’re mature enough where they can handle that, usually without sedation,” he said.
In Dr. Papsin’s practice, however, the vast majority of his patients are children. And for those younger patients, he noted, repeat procedures are problematic. “Most of them are going to need to be sedated for these scans, so you really want to avoid bringing them back for another scan,” he said. “That’s one of the main reasons why 90 percent of the children in our practice get both types of scans in one setting.”
Moreover, the two-scan strategy can be done with a minimum of logistical headaches and has some economic benefits as well. When children come in for an evaluation, “it’s cost-effective to get them into a CT testing area, give them the scan and literally wheel them down the hall to an adjacent room where we have an MRI set up,” Dr. Papsin explained. “It’s one visit, one sedation, and a very efficient way to diagnose their hearing loss and their readiness for implantation.”
Dr. Papsin said another benefit to doing both scans in one pre-operative visit is that once a cochlear device is implanted, undergoing a follow-up MRI is problematic because the scan’s magnetic field can pull out the metal component of the implant. “So this may be our only chance to get a baseline MRI image of the brain and the inner ear; having that is a huge help in subsequently managing these patients,” he said.


Another Study Yields Subtle Differences
Daniel Hajioff, FRCS, consultant ENT surgeon at University Hospitals Bristol in Bristol, United Kingdom, has also conducted a head-to-head trial of CT and MRI in the pre-operative imaging of CI candidates. But his reasons for doing the study offer an interesting counterbalance to Dr. Papsin’s approach.
“We had already been doing dual imaging in most of our pediatric patients,” he said. “But it really wasn’t working for us: It was expensive to order both tests, and we just weren’t sure the cost was justified by the added diagnostic information we were getting.” Moreover, “because our CT and MRI equipment were at opposite ends of our hospital for several years, trying to get both scans done in children while they were under the same general anesthetic was really proving to be difficult.”
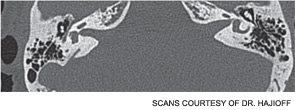
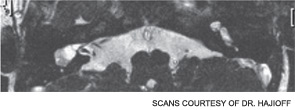
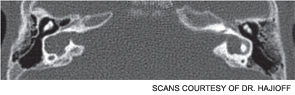
So Dr. Hajioff and his colleagues compared CT and MRI, hoping to determine whether one imaging modality was superior enough to become the imaging test of choice for most patients (Cochlear Implants Int. [published online ahead of print June 29, 2011). The study, which included 158 adults and children, found that both scans detected 44 significant abnormalities pre-operatively. Of those, 20 were considered critical to the selection of side for implantation, surgical procedure or decision to operate. MRI was able to detect all of those abnormalities (95 percent confidence interval [CI]: 0-2.3 percent). In contrast, CT alone missed 10 critical abnormalities (95 percent CI: 3.1-11.3). These findings were consistent in adults and children, the investigators reported.
“The simplistic conclusion from these findings would be that all comers should get MRI and that to save health care resources and minimize radiation exposure, we should forego CT scans,” Dr. Hajioff said. But, as convincing as the data are, real-world clinical situations often require a more nuanced approach, he added.
For example, although most of his adult patients only get an MRI, if there is a history of any prior surgery that might have altered the mastoid or if the patient has had meningitis, which can cause ossification, “we order a CT scan as well. It really is superior in imaging bone,” Dr. Hajioff said. “So we haven’t completely abandoned CT.”
Similarly, although MRI is slowly becoming the preferred option in children, adjunctive CT scans are still sometimes ordered. “But I am only [using CT] in cases where there is an increased likelihood that it might pick up something of interest, for example, kids with a history of severe infections, meningitis or craniofacial dysmorphic syndromes,” Dr. Hajioff said. “Those children get both scans in the same sitting.”
He added another reason why the study results favoring MRI shouldn’t be applied too aggressively, at least in children; like any clinical research, the study had some limitations. “Probably the biggest is the study size. Even though the number of patients [158] is larger than most previous studies, it’s still a relatively small sample. In our practice alone, we’ve probably done more than 500 implants. So larger numbers might have led to more robust—and perhaps different, although I doubt it—conclusions.”
What of the “old guard” of surgeons cited by Dr. Papsin, who tend to prefer CT scans as a sole imaging modality? “I don’t quarrel with that approach,” Dr. Hajioff said. “There are many surgeons who feel they need the roadmap of bony structures afforded by the CT scan in front of them before they operate. Personally, I am getting more comfortable not having that in place. Sure, you may not be able to see exactly where the facial nerve is, or see the sigmoid sinus in relation to other inner-ear structures, when you only order an MRI. But for me, the MRI tells you what you need to know; the rest of it you can work out while you are operating.”
Bottom line? “I think the CT scan, in some cases, is more of a psychological prop than an essential diagnostic tool,” he said.
MRI Gets Another Nod
Peter Roland, MD, professor and chairman of otolaryngology/head and neck surgery and professor of neurologic surgery at the University of Texas Southwestern Medical Center in Dallas, is also in the camp that favors MRI for certain patients and clinical settings. That stance, like those of Drs. Papsin and Hajioff, is based in part on a head-to-head trial of CT and MRI that Dr. Roland and his colleagues conducted in 56 children (Otol Neurotol. 2005;26:976-982).
“We found that MRI was more consistently able to identify types of abnormalities—for example, asymmetric nerve aplasia and cochlear obstruction—that were most likely to influence the implantation process,” Dr. Roland told ENT Today. Coupled with the fact that MRI is much more effective in identifying soft-tissue abnormalities in the inner ear, we felt that the study supported what we had known empirically for some time: that MRI is the superior scan,” Dr. Roland said.
He added that it’s not just the surgeons who prefer MRIs. “Most, if not all, of our pediatric neuroradiologists believe that they are better able to diagnose abnormalities of the cochlea itself using MRI than CT, and we use MRI preferentially for the evaluations of bilateral sensorineural hearing loss. That’s because the fluid signal is more revealing than the bone signal in terms of highlighting significant defects,” he said.
Are there some findings that CT can better elucidate? “Sure,” Dr. Roland said. “CT scans are great at letting you know whether a child has a normal oval or round window, which can complicate surgery.” Additionally, he noted, CT scans can better track the middle and mastoid course of the facial nerve. Thus, the scan is more useful in identifying and characterizing facial nerve anomalies, “but we have found that anomalous nerves are almost always associated with a malformed semicircular canal or vestibule, which are easily seen on MRI. If we identify either of these abnormalities on MRI, we get a CT, but that is very infrequent.”
It’s not surprising, therefore, that for the past five years, Dr. Roland and his colleagues at UT Southwestern have been using MRI almost exclusively to assess candidates for CI surgery. That approach works, he said, even in cases that involve severe inner-ear deformities. “If there is something significantly aberrant going on in the inner ear,” he explained, “the MRI will make that very clear to you, based on the absence of various types of fluid and air signals. It has to be a fairly subtle, and thus not really clinically significant, abnormality to be missed completely by the MRI.”
But he acknowledged that what works at UT Southwestern may not play in other hospitals or clinics. “I am associated with a children’s hospital that does five to ten MRIs on one-year-olds a day,” he said. ‘These kids have to be put to sleep in a sometimes-hectic scanning environment, and for us, that is absolutely routine. But that is decidedly not the case in many hospitals in the U.S., where putting a one-year-old to sleep for an MRI scan becomes a complicated business that is very uncomfortable for everyone involved.”
In such cases, in children who have not had meningitis and have some residual hearing, indicating that a nerve connects the cochlear cavity to the brain, “they are a clear candidate for a relatively uncomplicated cochlear implant, and for them, I think a CT scan is just fine,” Dr. Roland said. “I certainly would not be dogmatic and impose our preference for MRI on such a case.”
CT Scans in Select Patients
Andrew Fishman, MD, an otologist/neurotologist and skull base surgeon at the Feinberg School of Medicine, Northwestern University, Chicago, said choosing the best scan for evaluating CI candidates is not, at its heart, all that complicated: The decision should be based on the question of whether there are any cochlear-vestibular anomalies that preclude implantation. Or, stated a bit more simply, “Is there an adequate cavity that the implant can be successfully put in; are there nerves that are stimulable by the implant?” he said.
For the “vast majority” of adult patients, he said, CT scans can answer that question without the need for an adjunctive MRI. That is the case, he explained, because in most adults, the hearing loss is progressive, with no history of severe infections (such as meningitis) that would lead to scar tissue that shows up better on MRIs. Moreover, it’s rare for such patients to have otosclerosis or some other disease process that can actually physically obstruct the cochlea and require MRI to guide surgery.
For those reasons, “we start all of our adult patients on CT scans,” Dr. Fishman said. “Is it a solution for all patients? Of course not.” In fact, Dr. Fishman authored a recent review article that outlines the wide variety of possible cochlear-vestibular anomalies that can require adjunctive MRI scans (Otolaryngol Clin North Am. 2012;45:1-24). The more severe the malformation, he noted, the more helpful it can be to have MRI images guiding pre-operative evaluations. In one such condition, known as a common cavity, the cochlea and vestibule come together into a common rudimentary cavity. In one study cited by Dr. Fishman, common cavities accounted for 26 percent of the congenital inner-ear malformations detected (Laryngoscope. 1987;97:2-14). In such patients, he noted, “the canal that houses the auditory nerve is extremely narrow, and you really need an MRI to adequately visualize the nerve.” In such cases, he explained, MRI helps the surgeon determine which ear is the best option for receiving the cochlear implant. “The side that looks bigger—the one that will have the optimal nerve conduction—that’s the side you want to go after,” Dr. Fishman said. “You really can’t get that type of information from a CT scan alone.”
As for pediatric patients, “that’s a bit more complicated, but overall, factors such as a history of infection should definitely steer you towards MRI: It’s best at visualizing what’s going on inside the cochlea, whether it’s scarring or fluid build-up or other processes that can influence implantation,” he said.
As far as any ultimate answer to the question of which scan is best for pre-operative CI evaluation, “there really is no clear overall winner: It depends on the patient, any history that points to a potential cause for the hearing loss and also the surgeons’ comfort level with a particular scan,” he said.
Disclosures: Dr. Papsin disclosed that he is on the Speaker’s Bureau for the Cochlear Americas Corporation. Drs. Fishman, Hajioff and Roland had no relevant financial relationships to disclose.
Leave a Reply