Explore This Issue
September 2011The biggest gains in the future for surgical and therapeutic treatments of head and neck cancer will likely include the use of imaging techniques, radio-enhancers and drug delivery vehicles that are really, really small.
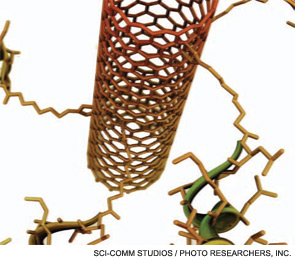
The first nanostructure, the “buckyball,” was created in 1985 from just 60 carbon atoms; elongated carbon nanotubes, which quickly found a place in composite materials, soon followed. In medicine, taking a cue from the hollow buckyball construct, the drug Doxil was created in 1995 by loading the chemotherapeutic doxorubicin within a lipid nanoparticle. To get an idea of nanomedicine’s scale, consider the fact that mammalian cells are typically 2,000-10,000 nm, and cellular organelles range from 100 to 300 nm, while nanoparticles are often 50 nm or less.
Surgeon and nanotechnologist Ivan El-Sayed, MD, associate professor in the department of otolaryngology-head and neck surgery at the University of California-San Francisco, just published a review of the topic as it relates to gold nanoparticles (Curr Oncol Rep. 2010;12(2):121-128). Dr. El-Sayed’s interest focuses on several potential applications, imaging in particular, and the nanoparticles in question are indeed made of gold. “Gold is very interesting because it has extraordinary optical properties,” he explained; it is able to scatter or absorb light, and, critically, both of these phenomena can be detected and are capable of providing in vivo information. Further, gold absorbs different wavelengths of light that, depending on the wavelength, may result in the particles giving off heat to the surrounding tissue or even ionizing radiation.
So what does this mean for head and neck cancer patients? The applications include tissue imaging, photothermal ablation of tissues surrounding a gold nanoparticle, radiation enhancement and drug delivery (an ability inherent to the scale of nanomaterials in general).
Taken in reverse order: A tumor-targeted gold particle coated with tumor necrosis factor alpha is currently the subject of a phase I clinical trial. For radiotherapy, due to gold’s absorption properties, “we could actually reduce the dose of radiation that we have to give to the patient,” Dr. El-Sayed said, “but still have effect at the tumor site, meaning that we might be able to re-radiate down the road.” Photothermal ablation of tissue is also a possibility, with the potential to overcome tumor drug resistance when used with chemotherapy.
Finally, consider imaging. “If you had a contrast agent to label the cells, that would really improve our ability to decide where to end the surgical margin,” which is extremely important not only for a cure, but also to reduce the impact of what can often be disfiguring procedures, Dr. El-Sayed said.
Key to the realization of these goals is successful targeting. “My day-to-day focus is to figure out how to functionalize the particles so that they can be used in these various biological applications,” Dr. El-Sayed said. Of the possible mechanisms to explore, the epidermal growth factor receptor (EGFR), a target that is over expressed in 90 percent of oral squamous cell carcinomas, seems the best bet. “The nanoparticles will still have to travel through a number of (physiologic) barriers to reach the target,” said Dr. El-Sayed. He’s convinced, however, that nanotechnology in head and neck cancer is not an “if” but a “when.”
 We could actually reduce the dose of radiation that we have to give to the patient.”
We could actually reduce the dose of radiation that we have to give to the patient.”
—Ivan El-Sayed, MD
When Is Now
For recent progress in targeted nanoscale therapy in head and neck cancer, look no further than the Journal of Oral Maxillofacial Surgery. (Ward BB, Dunham T, Majoros IJ, et al. Targeted dendrimer chemotherapy in an animal model for head and neck squamous cell carcinoma [published online ahead of print June 17, 2011].) The article describes a study conducted by Brent Ward, DDS, MD, and colleagues at the University of Michigan in Ann Arbor. Dr. Ward is an assistant professor and fellowship program director at the Michigan Nanotechnology Institute for Medicine and Biological Sciences and the department of oral and maxillofacial surgery at the University of Michigan.
“Whether head and neck surgeons or otolaryngologists or general surgeons, my colleagues all have an interest in limiting toxicity and in organ-sparing therapies,” said Dr. Ward, who thinks the nanotechnology platform being researched at his institute might be just versatile enough to fit the bill.
Dr. Ward is working with a multidisciplinary team of chemists, immunologists, biologists and physicists to develop dendrimers, which are 5 nm-diameter polyamidoamine, spherical constructs (the size of a hemoglobin molecule) that are amenable to multiple targeting moieties. “With this we have the ability to conjugate functional arms,” targeting folic acid receptors, EGFR or molecules sensitive to imaging modalities, for example, he said.
For therapeutics, “the power of this device is that we can look at a tumor, ID the receptors that are available and then target that specific tumor type based on its receptor availability,” he said. Heightened efficacy and reduced toxicity are the results.
In the current in vivo investigation, mice with tumor xenographs expressing a range of folic acid receptors, from high expression (cancerous) to mid-range to none (healthy tissue), were exposed to dendrimer particles spiked with multiple conjugates of the anti-folate drug methotrexate.
Because of the dendrimer’s ability to access the target, flowing through the smallest leak in the tumor’s leaky vasculature and bringing multiple chemotherapeutic molecules to bear, the construct was able to extend the survival of over-expressing mice. The reason? More drug reached and remained on target. “These are much higher doses than [are] being delivered in the free methotrexate realm,” said Dr. Ward, “and the more dose you can give the animal, the greater the effects are going to be—sort of a no-brainer. But despite the fact that we are giving much larger doses, the systemic toxicity that we are seeing is much less.”
According to Dr. Ward, once the methotrexate is attached to the device, it can’t get back out of the cell. “It tends to stay around the tumor longer and not be exported by the normal cellular mechanisms,” he said. If his theory is correct, dendrimer conjugates may be able to block the development of chemotherapy resistance.
With this proof of principle in hand, Dr. Ward and colleagues are looking toward the development of an EGFR construct (think, cetuximab) specifically intended to treat head and neck cancer. Hopefully, it will provide proof once again that good things do come in small packages. ENT TODAY
Leave a Reply