Chronic laryngitis is a multifactorial disease with a large differential diagnosis for the patient who presents with hoarseness. Fortunately, the diagnosis of inflamed larynx has improved in recent years.
Explore This Issue
September 2010Robert Sataloff, MD, professor and chair of otolaryngology-head and neck surgery at Drexel University College of Medicine in Philadelphia, said progress has included a growing understanding of the anatomy and physiology of the larynx; improved visualization with strobovideolaryngoscopy, videokymography and high-speed video; an improved understanding of laryngopharyngeal reflux (LPR); and the recognition of the role played by certain medications, such as steroid inhalers used for the long-term treatment of asthma.
Seth Dailey, MD, associate professor of otolaryngology-head and neck surgery at the University of Wisconsin in Madison, said gastric reflux multichannel intraluminal impedance testing, coupled with esophageal pH monitoring, has “allowed us to understand when there are reflux events up into the esophagus and whether they are liquid or non-liquid, acid or non-acid.” He added that “we can begin to understand if there is a strong, intermediate or weak correlation between those events and the patient’s symptoms,” which may aid decision for more aggressive therapy such as a Nissen fundoplication.
According to Dr. Dailey, the 24-hour pharyngeal pH probe has provided reliable enough measurements of pH pharynx secretions for otolaryngologists to gauge acid exposure.
“Within the last three years, the American Academy of Otolaryngology-Head and Neck Surgery has promoted more coalescent understanding of the unified airway,” said Kenneth Altman, MD, PhD, director of the Eugen Grabscheid, MD, Voice Center at Mount Sinai School of Medicine in New York. He cited the concept that aerodigestive disease is a multifactorial problem that can require collaboration with other specialists, such as pulmonologists, allergists and gastroenterologists.
Dr. Altman added that “if the patient doesn’t respond based upon empiric treatment from your clinical judgment, then objective tests are important to determine the underlying cause of chronic laryngitis. For example, if you’re thinking of acid reflux, a screening test would be a barium swallow, but a more objective test would be 24-hour impedance and pH probe,” he said. “If you’re thinking about upper respiratory disease, a screening test would be a RAST [radioallergosorbent test], but more formal evaluation would be by an allergist with a CT [computed tomography] scan of the sinuses.”
Adding to faster diagnoses is the availability of subspecialists. “I believe the biggest advance in recent years has been the creation of new voice centers and the training of new laryngologists, allowing for better delivery of voice care,” said Adam Klein, MD, assistant professor of otolaryngology-head and neck surgery at Emory University Voice Center in Atlanta.
Hot-Button Diagnosis
While otolaryngologists are gaining a better understanding of chronic laryngitis, the potential for overdiagnosis of LPR concerns some otolaryngologists.
“Reflux is often a cause of chronic laryngitis, but I think that we, as otolaryngologists, need to remember other potential causes,” said Dale Ekbom, MD, a laryngologist at the Mayo Clinic in Rochester, Minn.
Dr. Klein said the controversy relates to the frequency with which LPR is diagnosed. “It’s become a bit of a wastebasket diagnosis,” he said. “Unfortunately, it is often done without people doing a thorough workup to confirm or deny the presence of reflux.”
Lee Akst, MD, director of Johns Hopkins Voice Center in Baltimore, pointed to the side effects associated with proton pump inhibitors and other antacids. “These side effects get worse the longer someone is maintained on the medications,” he said.
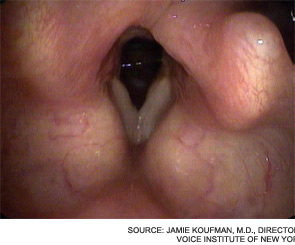
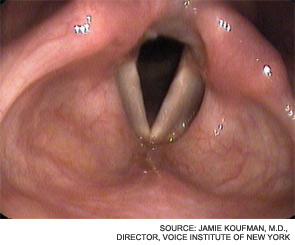
On the other hand, Jamie Koufman, MD, director of the Voice Institute of New York, professor of clinical otolaryngology at New York Medical College and author of Dropping Acid: The Reflux Diet Cookbook & Cure, said it is “profoundly disappointing that we are still in the Stone Age with regard to reflux, since it is one of the most important diseases of our time.”
Dr. Koufman pointed out some of the progress that has been made in this area. “Using state-of-the-art reflux-testing, we have shown that LPR accounts for 80 to 90 percent of laryngitis cases over a 25-year period,” she said. “The reflux conundrum today is primarily due to fragmentation between medical specialties, suboptimal diagnostic testing and treatment for LPR (at the hands of both otolaryngologists and gastroenterologists), and ignorance of the scientific literature on LPR. Many of my colleagues seem to have not even read the scientific articles.”
Linda Brodsky, MD, president of Pediatric ENT Associates in New York and co-author of a 2007 study on LPR (Int J Pediatr Otorhinolaryngol. 2007;71(9):1361-1369), said most physicians believe vocal cord nodules are the most common cause of hoarseness in children, “but I do not agree. I believe hoarseness is widely ignored by primary care physicians and parents…reflux laryngitis is the most common cause today.”
 “Reflux is often a cause of chronic laryngitis, but I think that we, as otolaryngologists, need to remember other potential causes.”
“Reflux is often a cause of chronic laryngitis, but I think that we, as otolaryngologists, need to remember other potential causes.”—Dale Ekbom, MD
Common Mistakes and Problems
For some patients initially seen by primary care physicians, accurate diagnosis and treatment may be delayed. That’s one reason AAO-HNS adopted guidelines for chronic hoarseness in September. [Visit enttoday.org to read a previous article on this topic, “Sore Spot: New hoarseness guidelines stir controversy.”]
Nonetheless, “chronic laryngitis is inflammation of the larynx; it is not commonly misdiagnosed,” Dr. Sataloff said. But, “its causes commonly are not recognized or are misdiagnosed because of lack of familiarity with some of the etiologies and suboptimal physical examination.” He added that most common mistakes are the results of an incomplete history and inadequate physical exam.
“Practitioners often attach the label of chronic laryngitis when they are unable to identify another cause,” Dr. Klein said. “Some people might be diagnosed with reflux when it is actually allergies, a vocal cord lesion or something worse. Therefore, it is important for patients to undergo a proper voice workup when their cause of hoarseness or laryngitis cannot be identified.”
Dr. Akst said many causes of chronic laryngitis relate to lifestyle rather than infection. “It’s often related to smoking, alcohol use, reflux disease, overuse of the voice [or] exposure to irritants like dust or chemicals or inhalers,” he said. “A lot of the treatment is in counseling patients how to take care of their voices and reduce inflammation.”
He added that another problem is looking only at structure and not function, such as muscle tension dysphonia. “In the absence of stroboscopy, the cords may look normal, with no lesions or paralysis, and the assumption is made that inflammation must be causing the voice complaints,” he said, noting that one role of fellowship- or subspecialty-trained laryngologists is to take that next step and look at vocal cord function.
And then there are the limitations of the sensory system. “As otolaryngologists, we are perpetually frustrated because of the sensory feedback from the esophagus and pharynx to the brain. If you have some sort of noxious stimulus in your throat, you might feel it in your ear,” Dr. Dailey said. “In addition to poor spatial resolution, temporal resolution is poor. The stimulus may have come and gone, but the patient still feels it.”
If misdiagnoses are occurring, Dr. Dailey said, it’s often due to the “general paucity of good diagnostic tools. In an ideal world, we could take biopsies and send them out for genetic analysis. Or maybe we could put stains on the pharynx so that we can see if there are pepsin molecules there. Until then, we’ll continue to have a best guess scenario.”

Leave a Reply