 Hair loss can be a significant issue for men over age 50. Androgenic alopecia affects an estimated 35 million men in the United States, and the National Institutes of Health estimates that more than 50% of men older than age 50 have some degree of hair loss. Women are not immune: The International Society of Hair Restoration Surgery estimates that 21 million women experience hair loss, affecting 50% of them by age 50.
Hair loss can be a significant issue for men over age 50. Androgenic alopecia affects an estimated 35 million men in the United States, and the National Institutes of Health estimates that more than 50% of men older than age 50 have some degree of hair loss. Women are not immune: The International Society of Hair Restoration Surgery estimates that 21 million women experience hair loss, affecting 50% of them by age 50.
Explore This Issue
October 2014Remedies for androgenetic alopecia do exist, but not many are approved by the U.S. Food and Drug Administration (FDA). Only two drugs, minoxidil and finasteride, currently have FDA approval for treatment of the condition. For women, minoxidil is currently the only FDA-approved treatment, although androgen inhibitors such as spironolactone and cimetidine are often used.
Two newer therapies involve platelet-rich plasma injectables and the use of robotics to enhance follicular unit extraction during hair transplantation. These treatments have benefits and drawbacks for otolaryngologists wishing to expand their hair restoration clinical practice.
Platelet-Rich Plasma Injections
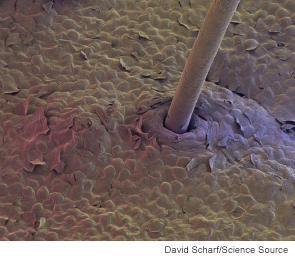
Platelet-rich plasma (PRP), which can also be found in the form of a platelet gel, is a type of blood plasma that has been enriched through concentration of autologous platelets. PRP is used in clinical practice to stimulate bone and soft tissue healing in a number of medical treatments for cardiac muscle injury, bone repair and regeneration, nerve injury, plastic surgery, and more. PRP treatment is not a replacement or an alternative to another hair restoration therapy; rather, it fills a gap in treatment modalities.
Physicians are using PRP in the treatment of androgenic alopecia both on its own and as an adjunct to hair transplantation surgery, said Lisa Ishii, MD, associate professor of facial plastic and reconstructive surgery in the department of otolaryngology-head and neck surgery at Johns Hopkins Medicine in Baltimore. “Some physicians inject it directly into the scalps of patients who have androgenic alopecia and who have existing hair follicles to stimulate hair growth,” she said. “The same injection technique is used to try to promote hair growth in patients who have undergone hair transplantation surgery.”
“Doctors are using it for various indications such as chronic tendinopathies and arthopathies, arterial leg ulcers, pressure ulcers, chronic wounds, burn, surgical wounds, post-traumatic scars, and facial rejuvenation,” said Gorana Kuka, MD, chief resident at Colic Hospital, the largest private hospital for plastic, reconstructive, and aesthetic surgery in Serbia. “Due to the many different growth factors that are released after platelet degranulation, PRP initiates and enhances physiological processes that contribute to tissue recovery.”
By adding growth factors into the scalp, said Dr. Kuka, the idea is to “wake up” dormant stem cells that every hair follicle contains, to trigger cell division of the hair matrix and to reduce persistent inflammation.
For those patients recovering from surgery, PRP can be used to promote wound healing. “When a patient has had hair transplantation, there are thousands of tiny wounds all over the scalp,” said Dr. Ishii. “Some physicians have also used PRP injections for patients with alopecia areata, which is a more scarring form of hair loss.” PRP injections may be of benefit to patients who have undergone hair transplantation in scalp skin that has been damaged through radiation or reconstructed through a skin graft.
The use of PRP injections is still new enough—within the last few years—that data are still being gathered. “I don’t believe the current data are convincing, but that may not be because it doesn’t work,” said Dr. Ishii. “There really haven’t been many large clinical studies on PRP’s particular use in hair restoration. I’ve spoken with colleagues across the country and around the world, and the evidence is still quite anecdotal.”
Dr. Ishii remains optimistic about PRP’s use in hair restoration. “I believe that once the effects are studied more formally, we will see that it does have a benefit,” she said. “PRP use is more established in other areas—we have some data in wound healing with facial rejuvenation surgery, for example, and there are data from the orthopedic literature that notes that PRP does contribute to faster wound healing. Translating that to the fact that its use, particularly in connection with hair transplantation, is another wound healing episode, it makes sense that there would be some benefit.”
In Dr. Kuka’s experience, patient satisfaction has been high when treated with PRP. “The feedback that I have had so far was that the hair loss either slowed down or stopped, with as much as 20% to 30% regrowth achieved. I have also treated patients with alopecia areata and, recently, one with alopecia totalis who started noticing some hair regrowth after four years of being without hair.”
Robotic Hair Transplantation
Surgical hair restoration is a thriving medical practice, with estimated worldwide revenue of approximately $1.87 billion U.S. (International Society of Hair Restoration Surgery).
There are two main methods for harvesting follicles for hair transplantation: strip harvesting and follicular unit extraction (FUE). During strip harvesting, a strip of skin is excised from a patient’s scalp and cut into individual follicular units. During follicular unit extraction, naturally occurring groups of one to four hairs in a follicle are removed individually from a section of donor scalp skin.
Both methods have benefits and drawbacks. FUE generally has a shorter recovery time than strip harvesting and does not leave a linear scar; it also allows for finer hair to be harvested and is a beneficial choice in situations when the scalp is too tight for a strip incision to be feasible; however, FUE is done over a much larger area than strip harvesting, so hair thinning in harvested areas is a possible aftereffect.
Robotic devices for hair restoration were initially discussed as far back as 2007. In 2011, the ARTAS Robotic System received FDA clearance for performing FUE to harvest hair follicles from the scalps of men diagnosed with androgenic alopecia. The unit uses an image-guided robotic arm, special imaging technologies, small dermal punches, and a computer interface to harvest individual follicle units for transplantation.
Benefits to using a robotic surgical unit include increased speed and precision, the ability to set key parameters such as depth, and a lower possible error rate due to physician fatigue.
Dr. Ishii isn’t convinced that the use of robotics to achieve FUE is necessarily more beneficial, however. “The real disadvantage to strip harvesting is that it leaves a scar on the back of the scalp,” she said, “but it’s a very low-morbidity procedure, and any scar is concealed by remaining hair. A scar would be a concern to a patient who wears his hair very short to the scalp or who decides to throw in the towel and shave his scalp completely bald. When placing the roots in the recipient area, there is no reason for me to think that a robot will be able to do it with higher precision than humans who are expert at performing the surgery.
Dr. Kuka agreed, although she does see some benefit to using robotics. “I support the idea of having a robot doing a surgical procedure, but I don’t believe the time for it has come yet,” she said. “I believe the device itself has some deficiencies that need to be resolved before we can say that what it is doing is equal to or better than what can be done by an experienced doctor.”
Future Possibilities
Although there are no other new procedures in clinical use at this time, Dr. Ishii and Dr. Kuka do see some interesting technology for hair transplantation in development.
Hair root culturing. Dr. Ishii believes that there are studies currently underway with developing hair roots in culture. “Let’s say that a patient wants a hair transplant but doesn’t have a lot of hair left anywhere,” she said. “With this technology, we could take out five of that patient’s hair roots, and in culture, turn them into 5,000 hair roots. I believe this is definitely on the horizon, but I don’t know how far off on the horizon.”
Regenerative medicine. Dr. Kuka strongly believes that advances in regenerative medicine have potential applications in hair restoration. “Research is currently examining the use of stem cells to regenerate damaged or diseased tissue in many conditions such as heart disease, Parkinson’s disease, spinal cord injury, arthritis, burns, and scleroderma,” she said. “I believe fat grafting and the use of stem cells will be key in treating hair loss in the near future.”
3-D hair root printing. Researchers are expanding the use of biomedical 3-D printing technology in other areas of medicine, including 3-D printing of internal organs and skin. Dr. Ishii foresees the ability to print 3-D hair roots, eliminating the need for a donor area entirely and giving hair transplant surgeons an unlimited supply; however, although private companies are currently developing this technology further, its clinical use for hair transplantation is still in the distant future.
Amy Eckner is a freelance medical writer based in California.
Leave a Reply