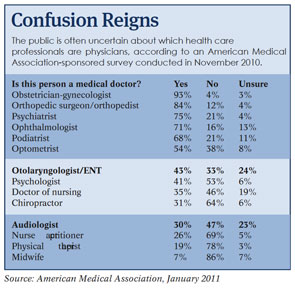
More often than not, members of the public are confused about which health care providers are physicians and which are not. That uncertainty is expected to increase as the trend toward non-physician providers earning doctorate degrees continues and as demand for services grows with the millions of people gaining insurance under the 2010 health reform law.
Explore This Issue
July 2011Federal legislation offered in the House of Representatives aims to help reduce the confusion by ensuring that providers properly identify themselves in marketing materials. The bill would prohibit health care professionals from making statements or engaging in acts that misrepresent their education, training, degree, licensing or clinical expertise.
The measure, the Healthcare Truth and Transparency Act of 2011, has broad support in the physician community. In March 2011, 67 state and national medical societies sent a letter of support to the bill’s sponsors, Reps. John Sullivan (R-Okla.) and David Scott (D-Ga.).
Patient Uncertainty
“Recent studies confirm increasing patient confusion regarding the many types of health care providers, including physicians, technicians, nurses, physician assistants and other allied providers, engaged in providing services in the health care setting,” the letter stated. “Ambiguous provider nomenclature and related advertisements and marketing are exacerbating patient uncertainty.”
Physician supporters of the legislation point to a recently released American Medical Association-sponsored survey of 850 adults. The survey found, for example, that 30 percent of respondents believe audiologists are medical doctors, and only 43 percent correctly identified otolaryngologists as physicians.
The fact that many patients don’t know that otolaryngologists are physicians is “very frightening,” said Paul M. Imber, DO, chairman of the American Academy of Otolaryngology-Head and Neck Surgery (AAO-HNS) Legislative Representatives Committee and member of the AAO-HNS Board of Governors Executive Committee. “But what is even more of an issue is that a lot of people are out there marketing themselves as doctors, and they are doctors by degree but not physicians. It can be very confusing to the public.”
Truth in Advertising
If passed, the legislation would make such practices a violation of the Federal Trade Commission Act. It would hold all health care providers “to the same truth in advertising standards as every other good or service in the United States,” according to a press release from the office of Rep. Sullivan.
A range of organizations representing mid-level practitioners, including the American Academy of Audiology, oppose the bill. In a February 2011 letter to House lawmakers, these 11 organizations argued that the measure is unnecessary because the issue is “already well regulated by the states and other agencies.”
But the measure’s proponents said the Accountable Care Act of 2010 makes the truth in advertising bill more critical than ever. “The new health insurance law will open the door to millions of new patients to join the health care system,” Rep. Scott stated in a news release. “This means that thousands of new health care professionals need to be trained annually to address the increased demand for services. Health consumers should be empowered to make decisions based on accurate information about their service provider.”
Already, the federal government is the nation’s biggest insurer, Dr. Imber noted. Once the reform law is in full effect, its broadened Medicaid eligibility provisions would mean that more people would be covered by the program. In addition, the Medicare population will burgeon as 76 million baby boomers age into the program. The first 2.5 million of this generation reach eligibility this year.
“When it’s actually the federal budget that’s involved, the federal government needs to know that the dollars are being spent in appropriate places,” Dr. Imber said. “The services provided must be appropriate, delivered by the appropriate providers. Patients need to be assured that they are getting the best care by the best people, and the government needs to be assured that it is getting the best bang for the buck.”
Lawmakers need to understand the differences between otolaryngologists and audiologists, Dr. Imber said. “Audiologists aren’t trained—nor is it part of their scope of practice—to be involved in the diagnosis and management of otological disease.” The truth and transparency legislation would help clarify the matter for everyone, he added.
The legislation specifies that it would not affect state laws regarding the scope of practice for the various non-physician providers. Many of the practitioners who have not traditionally earned advanced degrees are getting them now, noted AAO-HNS President J. Regan Thomas, MD. “Everybody should be proud of their degree and proud of that advanced training,” he said. At the same time, “they should feel very comfortable making sure that everyone understands what their background is and what their area of expertise is.”
Dr. Thomas heads the department of otolaryngology-head and neck surgery at the University of Illinois, Chicago, where all of the audiologists have doctorate degrees. The department’s audiologists make their expertise clear to avoid confusion among patients, Dr. Thomas said.
The federal legislation, if passed, would build on similar laws adopted in a handful of states, including Arizona, California and Illinois. The Illinois law, passed in 2010, also requires health care professionals to wear name tags that identify their licenses, as does a similar Pennsylvania law. Despite some success at the state level, federal legislation is necessary because the confusion among patients is pervasive nationwide, Dr. Imber said.
New Momentum
Although similar bills have failed in Congress in years past, otolaryngologists are hopeful this time around. The support of so many physician organizations has given the legislation momentum, Dr. Thomas said. The AMA survey also indicates backing among the public. Eighty-seven percent of respondents said they’d support a measure requiring all health care advertising materials to clearly designate the level of education, skills and training of the providers promoting their services.
“It just makes sense and would be appropriate for the public,” Dr. Thomas said.
Leave a Reply