Dr. Sowerby said the process of obtaining informed consent has four main components, as established in the landmark legal decision Schloendorff v. Society of New York Hospital (1914). According to this decision, to give consent, a patient must understand the following:
Explore This Issue
January 2017- The nature of the disease or condition;
- The benefits and the risks of the procedure;
- The alternatives to the procedure; and
- The consequences of no action.
Dr. Sowerby acknowledged that it can be tough in a busy practice to have a thorough discussion of all of those components with a patient, to the point where you’ve answered his or her concerns. “As an example, we all have our little spiel that we give when we take consent for a specific procedure. … If you’re a patient and you’re hearing that and you hear “heart attack,” and you get stuck on heart attack, you miss all of the other stuff that’s discussed during that consent. And you end up signing the piece of paper because you know you have five or 10 minutes with the physician. But you may not have had all of your concerns addressed, and you definitely don’t remember everything that was discussed.”
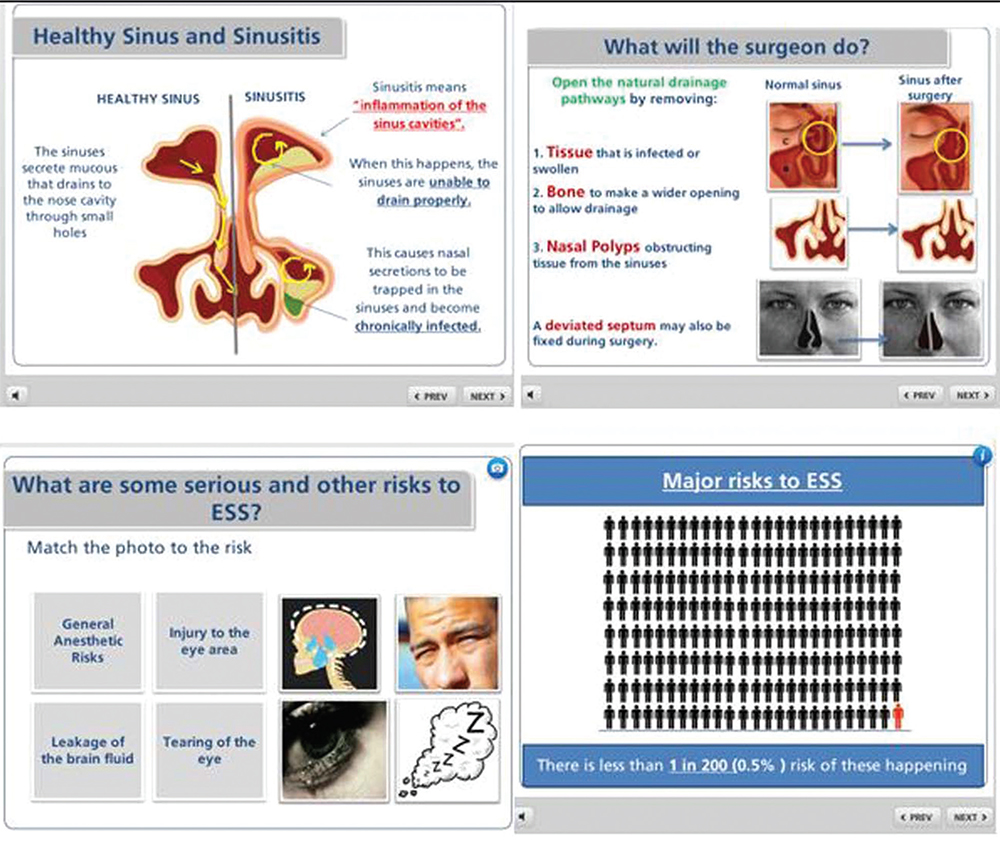
In June 2016, Dr. Sowerby and his colleagues published a paper in The Laryngoscope on the process of informed consent for ESS (Laryngoscope. 2016;126:1273–1278). The researchers found an early improvement in overall risk recall in patients who finished an interactive multimedia module (see Figure 1). The report concluded that it is important to integrate multimedia tools into the otolaryngologist’s armamentarium for clinical practice. “Simple, interactive multimedia education modules offer a cost-effective, efficient, and effective platform to supplement the traditional informed consent process,” they concluded.
(click for larger image)
Figure 1. Screenshots of Dr. Sowerby’s multimedia module for patient consent. Audio voice-over, images, and relevant figures were synchronized to convey clinical information. Animations were used to describe visual phenomena. To optimize patient comprehension, the module contained information at the eighth grade level and incorporated large fonts, bulleting, bolding, and underlining, as well as graphic displays using pictographs of risks and benefits. The module was designed to be interactive to let the patient control the information flow rate.
Credit: The Laryngoscope. ©The American Laryngological, Rhinological and Otological Society, Inc.
“The thing I like about the multimedia slideshow we have created is that it gives us control of what patients are seeing,” Dr. Sowerby added. “Sometimes patients don’t feel duly informed, and if they don’t, they’re going to do a Google search, and they’re going to see what shows up there, and they may or may not be reading things that are A) factual or B) realistic to their specific case. So, having some control over that, I think, is beneficial. It lets us ensure that the discussion is [going] in the direction it needs to be for that specific patient.”
Putting Patients at Ease
Zara Patel, MD, assistant professor of otolaryngology-head and neck surgery and an expert in advanced endoscopic sinus and skull base surgery at Stanford University School of Medicine in Palo Alto, Calif., said that while patients want to know the risks of a procedure, it is incumbent on otolaryngologists to deliver the news in a way that avoids overly medical terms and minimizes anxiety. Of course, that conversation can be particularly difficult with rhinology procedures that involve operating in proximity to the brain and eyes.