Explore This Issue
February 2014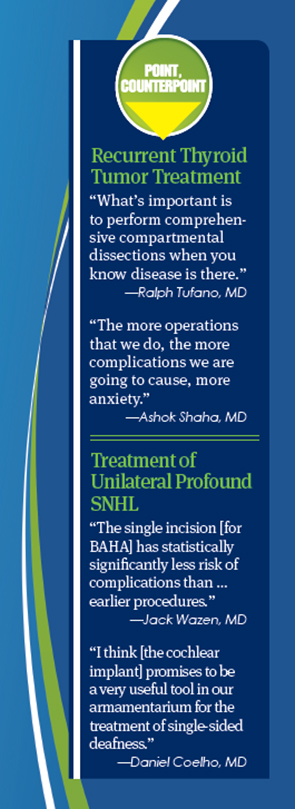
Experts came together in a session entitled “The Great Debate-Point/Counterpoint” to discuss treatment of recurrent thyroid tumors and unilateral profound sensorineural hearing loss in a “debate.”
Recurrent Thyroid Tumors
Whether recurrent thyroid tumors always require surgical treatment is a question without a firm answer, but two experts in the field offered their views during the session.
Ralph Tufano, MD, director of the Johns Hopkins Hospital Multidisciplinary Thyroid Tumor Center in Baltimore, supported a more aggressive approach. The medical literature, he said, shows that in cases where the physician knows there is disease in the central neck or the lateral neck upon initial presentation—disease that’s “clinically apparent”—the median recurrence rate is 22%, a figure he calls “almost shameful” to surgeons.
“The onus is on the surgeon to clear that disease whether it is primary or recurrent/persistent and not rely on radioactive iodine or additional treatment,” Dr. Tufano said. “What’s important is to perform comprehensive compartmental dissections when you know gross nodal disease is there.”
But Ashok Shaha, MD, professor of head and neck surgery at Memorial Sloan-Kettering Cancer Center in New York City, said observation is the right course in many cases. “If you have a small recurrence in a low-risk patient where the survival is 99%, do we need to go back and take care of the patient when the tumor is less than 1 cm?” he said.
Sometimes, the disease will not even be found, and there is a risk of complications, he added. Today’s technology allows for the discovery of micro-recurrent disease, but this doesn’t make the patient a surgery candidate. “Patients with multiple positive nodes from papillary cancer may have additional nodes in the paratracheal area and may never come out of mild hyperthyroglobulinemia,” said Dr. Shaha. “That does not mean all of them will require surgical intervention. They can live very happily with mild hyperthyroglobulinemia.” Approximately 20% to 30% of patients will have a recurrence, but almost half of those will remain with mild hyperthyroglobulinemia.
Dr. Tufano responded that, in the right hands, there is a greater likelihood that the nodule recurrence will be found in surgery if a compartmental resection is performed. “We’re not talking about a low-risk patient every time; we’re not talking about only sub-centimenter disease,” he said. “I don’t think that in this situation we can count on every tumor to behave accordingly to the low-risk profile. And we don’t know which ones will be aggressive and which ones will remain relatively indolent and quiescent.” Having a patient get lost to follow-up, only to have a serious recurrence four or five years later, can be disastrous, he said.
Technology is evolving and, eventually, otolaryngologists might be able to determine which tumors require immediate surgery. “Until that day comes and until we have more concrete evidence…. it’s incumbent upon the surgeon to treat this disease accordingly,” said Dr. Tufano.
Dr. Shaha said that a plan developed through meetings between the surgeon, endocrinologist, and the patient is crucial, so that patients are not lost to follow-up. “The more operations that we do, the more complications we are going to cause, more anxiety,” he said. “What we need is an understanding between the surgeon, the endocrinologist, and the patient himself, that we have a strategy. The problems come when there’s a dichotomy of opinion between the surgeon and the endocrinologist. And the endocrinologist says, ‘Yes, they have cancer, go in and have surgery.’ The surgeon doesn’t want to operate. And what does the endocrinologist do? Send the patient somewhere else…. Let the treatment not be worse than the disease.”
BAHA v. Unilateral Devices
In another “debate” during the session, Jack Wazen, MD, director of research for the Ear Research Foundation at the Silverstein Institute in Sarasota, Fla., discussed bone-anchored hearing devices, and Daniel Coelho, MD, assistant professor of otology, neurotology, and skull base surgery at Virginia Commonwealth University in Richmond, talked about unilateral cochlear implants.
Dr. Wazen said that research has shown that the newer, single-incision approach for implant bone-anchored hearing aids (BAHA) is a safer approach. “We’ve confirmed that the single incision has statistically significantly less risk of complications than the dermatome or the other earlier procedures,” he added.
With the DermaLock system, the abutment is covered with hydroxyapatite, with the intention of soft tissue adhering to it and creating a better seal, making for less soft-tissue inflammation and fewer complications. This is now FDA-approved, and the procedure takes approximately 10 minutes. Other systems are the Sophono, without a skin-penetrating abutment; the SoundBite Hearing System, which uses a wireless microphone behind the ear and a device that transmits through the teeth; and the Attract System, which has a magnetic system and no skin-penetrating abutment.
Dr. Coelho described the benefits of unilateral cochlear implants, which are not yet FDA-approved. Since they don’t have to route sound through the normal-hearing ear, they give patients two sides with hearing, rather than just one. The benefits of bilateral hearing, he said, are well borne out in studies, with better ear-specific hearing results when compared with BAHA and contralateral routing of offside signals devices, particularly with respect to sound localization and hearing amid noise.
He added that it is important to consider the best option for the patient per ear. “Cochlear implants for single-sided deafness may not always be the best option,” he said, “In our clinic, everybody gets trialed with the other devices first. There are many outcomes that still have to be studied and many factors that we have to consider prior to mainstream acceptance of CI for single-sided deafness.”
“We’re in the early stages of this now here in this country, but I think it promises to be a very useful tool in our armamentarium for the treatment of single-sided deafness, especially in patients with severe tinnitus.”
Leave a Reply