Explore This Issue
February 2014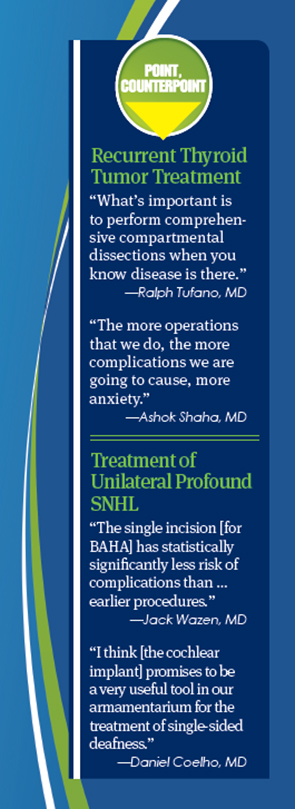
Experts came together in a session entitled “The Great Debate-Point/Counterpoint” to discuss treatment of recurrent thyroid tumors and unilateral profound sensorineural hearing loss in a “debate.”
Recurrent Thyroid Tumors
Whether recurrent thyroid tumors always require surgical treatment is a question without a firm answer, but two experts in the field offered their views during the session.
Ralph Tufano, MD, director of the Johns Hopkins Hospital Multidisciplinary Thyroid Tumor Center in Baltimore, supported a more aggressive approach. The medical literature, he said, shows that in cases where the physician knows there is disease in the central neck or the lateral neck upon initial presentation—disease that’s “clinically apparent”—the median recurrence rate is 22%, a figure he calls “almost shameful” to surgeons.
“The onus is on the surgeon to clear that disease whether it is primary or recurrent/persistent and not rely on radioactive iodine or additional treatment,” Dr. Tufano said. “What’s important is to perform comprehensive compartmental dissections when you know gross nodal disease is there.”
But Ashok Shaha, MD, professor of head and neck surgery at Memorial Sloan-Kettering Cancer Center in New York City, said observation is the right course in many cases. “If you have a small recurrence in a low-risk patient where the survival is 99%, do we need to go back and take care of the patient when the tumor is less than 1 cm?” he said.
Sometimes, the disease will not even be found, and there is a risk of complications, he added. Today’s technology allows for the discovery of micro-recurrent disease, but this doesn’t make the patient a surgery candidate. “Patients with multiple positive nodes from papillary cancer may have additional nodes in the paratracheal area and may never come out of mild hyperthyroglobulinemia,” said Dr. Shaha. “That does not mean all of them will require surgical intervention. They can live very happily with mild hyperthyroglobulinemia.” Approximately 20% to 30% of patients will have a recurrence, but almost half of those will remain with mild hyperthyroglobulinemia.
Dr. Tufano responded that, in the right hands, there is a greater likelihood that the nodule recurrence will be found in surgery if a compartmental resection is performed. “We’re not talking about a low-risk patient every time; we’re not talking about only sub-centimenter disease,” he said. “I don’t think that in this situation we can count on every tumor to behave accordingly to the low-risk profile. And we don’t know which ones will be aggressive and which ones will remain relatively indolent and quiescent.” Having a patient get lost to follow-up, only to have a serious recurrence four or five years later, can be disastrous, he said.
Leave a Reply