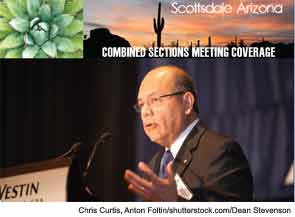
SCOTTSDALE, Ariz.—The educational environment is changing, “perhaps more drastically than ever before,” and the otolaryngology community may not be doing enough to face these changing times, said Jesus Medina, MD, FACS, in his presidential address to the Triological Society here on Jan. 24 as part of the organization’s Combined Sections Meeting. Click here to listent to the entire Presidential Address.
Restrictions on training hours and a changing culture with more emphasis on personal time and increased family responsibilities has put a strain on the education of residents, a strain that calls for taking immediate steps to improve how residents are trained, said Dr. Medina, professor of otorhinolaryngology at the University of Oklahoma Health Sciences Center in Oklahoma City. “Resident work hour regulations were long overdue, they’re here to stay and they’re likely to be reduced further in the future,” he added.
Unfortunately, the pinch on training hours has come as the amount of material to be learned has increased, and more demands on educators has had an impact on how residents are taught, he said.
“It is undeniable that the motivation and enthusiasm to teach have been diminished by the pressure of faculty time that results from a heavy burden on patient care, by the increasing need to rely on clinical productivity to ensure an adequate income and by the fact that it is becoming increasingly more difficult to teach surgical skills by practicing on patients,” he said.
Solutions
In the face of these changes, Dr. Medina offered the following recommendations:
Change the training schema in otolaryngology. He proposed that the fourth year of medical school could be used toward the first postgraduate year. This would give the student a jumpstart on obtaining the knowledge and skills needed for residency. Some of the rotations of the first residency year, such as emergency medicine, could easily be covered in the fourth year of medical school, he added. While this would take time to implement, it would be a worthwhile endeavor, he said, adding that this would provide a better transition into residency and increase the time available for training.
Guide residents so that they can maximize the efficiency of their learning. Research has shown that almost half of otolaryngology residents exhibit a “convergent learning style,” meaning that they learn best by doing tasks with help from a supervisor when needed, he said. “For these individuals, didactic lectures and brainstorming sessions are not useful. Intuitively, then, helping each resident identify how he or she learns best would be useful,” he said. “We need to stop forcing everyone to attend our lectures…. That 45 percent of residents with a convergent learning style cannot afford to daydream through lectures and then have to find another time that they can learn their own best way.”
Expand learning opportunities. Dr. Medina proposed a departure from the traditional lectures and tutorials “that are often held at an inflexible time and in a uniform way” and a move toward a variety of learning techniques, including e-learning. While acknowledging that this change is taking place now, Dr. Medina thinks it isn’t progressing fast enough. “Doing this can go a long way toward easing the pressure on time for both the clinicians trying to impart their knowledge and the residents trying to acquire it,” he said. “We must also develop training opportunities outside the operating room using simulators, artificial body parts and animal models.”
Maximize the effectiveness of teaching. Teaching might come naturally to some people, but this is not true of most, he said. “Regardless of our basic ability, the preparation to teach occurs as on-the-job training by trial and error,” he added. “Unfortunately, this type of preparation is empiric, usually takes a long time and often results in a rigid learning style…. We can no longer afford this type of preparation.”
Educating the Educators
Dr. Medina called for a “required systematic effort that leads clinicians to understand the latest developments in education theory and practice and to correlate them into a training program.” He said the Triological Society needs to take a role in “educating the educators” by working with the Otolaryngology Program Directors Association and the Society of University Otolaryngologists, and said steps have already been taken to make that happen.
For guidance, he pointed to the trainer’s course of the Royal College of Surgeons of England, a program that acknowledges differences in learning styles and the implications of these differences on how students should be educated, emphasizes the ability to relate areas of learning to surgery and covers the advantages and disadvantages of different teaching methods. “The end product of this type of educational program is a knowledgeable, open-minded and flexible teacher who knows about, and is not afraid to try, different proven techniques or methods of teaching.”
Leave a Reply