Patterns of Inflammation
The potential to identify specific molecular biomarkers of CRS to individualize treatment is being advanced through research on CRS endotyping, through which investigators are looking at the patterns of inflammation in the tissue of nasal polyps in people with CRS. “We still rely on phenotypes in the clinic,” said Dr. Kern, “but we can gaze at the future in terms of endotyping.”
Explore This Issue
July 2019A recent study by Dr. Kern and colleagues that looked at the presence of subsets of innate lymphoid cells (ILCs) found that the subset ILC2 may play an important role in the development of type 2 inflammation found in patients with CRS and nasal polyps (Immun Inflammation Dis. 2017;5:233–243). In the study, the investigators used multiple techniques to look at the presence of subsets of ILCs in patients with CRS, both with and without nasal polyps. ILCs, along with T-helper lymphocytes, produce high levels of cytokines that are present in distinct patterns in the tissue. These patterns will likely define the clinically relevant endotypes, each of which will respond differently to current treatment options. Type 2 inflammation, defined by the presence of elevated type 2 cytokines (IL-4, 5 and 13), is present in the vast majority of patients with CRS with nasal polyps. This Type 2 endotype—or, more likely, a group of related type 2 endotypes—has been particularly difficult to treat, with a high recurrence rate after both medical and surgical therapy. Type 1 and Type 3 inflammations are less common and likely more responsive to treatment. In CRS patients without polyps, the inflammation is more heterogeneous, but a large percentage still exhibit Type 2 inflammation.
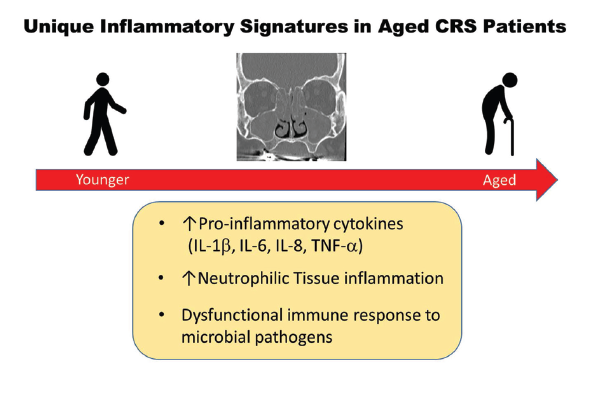
Figure 1. Unique Inflammatory Signatures in Aged CRS Patients.
Reprinted from J Allergy Clin Immunol. 2019;143:990–1002, Copyright 2019, with permission from Elsevier.
According to Dr. Kern, each pattern of inflammation will likely respond differently to various treatment options in ways that should be predictable. “We are still working this out,” he said, emphasizing that the research is only relevant if it has clinical application—that is, if it can shed light on the natural history of the disease, help predict who will respond to what treatment, and determine which patients will do well on a given treatment.
For Dr. Kern and others, this is the direction in which CRS treatments are heading. “In the future, we will be able to subdivide patient groups more precisely, and that will lead to rolling out precision, personalized medicine in which we can really predict from mucus or a blood sample how to treat patients,” he said.
Underscoring the need for further research is the emergence of biologic agents that can target specific mechanisms of disease, a treatment already used for patients with asthma. This advance is on the doorstep for patients with CRS. Dr. Kern pointed to results of a study recently presented at the American Academy of Allergy, Asthma and Immunology (AAAI) meeting in February 2019 that showed the safety and efficacy of the biologic agent dupilumab for nasal polyps (“Efficacy and safety of dupilumab in patients with chronic rhinosinusitis with nasal polyps: results from the randomized phase 3 SINUS-24 study”).
According to Dr. Kern, the biologic agent will hopefully gain approval from the Food and Drug Administration for treatment of nasal polyps sometime later this year, representing a major advance in the ability to manage patients with severe CRS with nasal polyps.