In mid-February, the Joint Commission introduced a new online tool meant to help combat inconsistencies in the surgical time out process.
Explore This Issue
March 2012To access the tool, health care providers must log in to the Targeted Solutions Tool (TST) website (jointcommissionconnect.org), where they can review a list of events that should occur before an incision is made. The aim is to prevent a cascade of errors that can begin before a patient is wheeled into the operating room.
Project Leader Melody Dickerson, RN, MSN, said the tool is meant to help organizations measure risk across their surgical system, including scheduling, pre-operative and operating room areas. The tool assists in monitoring surgical cases for weaknesses that could result in wrong-site surgeries, she said. “Most organizations are really proud of their OR on-time start records,” she said. “Yet most don’t have a policy in place to ensure that the necessary documentation is available when the patient arrives for surgery.”
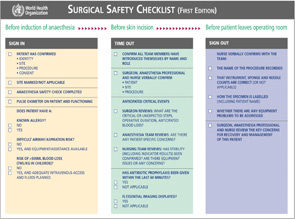
Since the Joint Commission released its Universal Protocol regarding this issue in 2004, hospitals have made refinements to their time outs in order to reduce the incidence of wrong-site, wrong-procedure and wrong-person surgery.
Variation
Hospitals, ambulatory surgical centers and health systems are tailoring time outs to their specific needs, and otolaryngologists in various subspecialties must conform to these regulations.
“Most surgeons working in hospitals really don’t have a choice as to how they do time outs. It typically is an OR or hospital standard,” said Michael M. Johns III, MD, associate professor of otolaryngology at Emory University School of Medicine and director of the Emory Voice Center in Atlanta.
In formulating these policies, however, hospital administrators do seek input from surgeons, anesthesiologists and nurses. While this sets a minimum standard, health providers can go above and beyond the basics to ensure safety.
“I think it’s important, as part of the time out, not to just review who the patient is, what the surgery is, what the planned procedure is, but also to make sure that all the critical equipment that’s needed for the case is functioning before you start,” Dr. Johns said.
Ideally, the dialogue should cover anticipated blood loss and other complications. “If you review those additional things beforehand,” he said, “then you’re less likely to have errors. It doesn’t take a lot of time to do this. It really is a one-minute-or-less procedure.”
Time outs are typically done with the surgeon and the circulating nurse confirming the patient’s name, side of the surgery, exact procedure and proper body positioning. The scrub nurse, scrub technician and anesthesiologist are also included. If they do not agree on all these pieces of information, the process is halted until resolution occurs.
Leave a Reply