INTRODUCTION
Bilateral vocal fold paralysis (BVFP) is an uncommon congenital anomaly resulting from disruption of the nerve supply to the muscles of the larynx that typically presents at birth with upper airway symptoms such as stridor, chronic respiratory insufficiency, dysphagia, and respiratory distress. The etiology of this condition varies; while most cases are idiopathic, BVFP can also be the result of injury related to cardiac procedures, neurogenic disease, birth trauma, or other causes (Otolaryngol Clin North Am. 2008;41:889-901). Congenital BVFP reportedly accounts for 30% to 62% of cases of pediatric vocal cord paralysis, and can be associated with substantial upper airway obstruction requiring urgent surgical intervention in 50% of patients (Otolaryngol Head Neck Surg. 2002;126:349-355).
Explore This Issue
November 2021Historically, congenital BVFP was managed with tracheostomy to secure a stable airway and subsequent expectant management in anticipation of spontaneous resolution of the condition. Though previous studies of children with BVFP have shown that the majority of patients undergo tracheostomy for initial management of this condition, it is important to note that tracheostomy is a procedure associated with high morbidity and mortality, and should be avoided if possible (Int J Pediatr Otorhinolaryngol. 2020;138:110325). More recent studies have identified congenital BVFP management methods that succeed at securing airway patency while avoiding the need for a tracheostomy. These procedures include, but are not limited to, cricothyroid botox injection, vocal cord lateralization, arytenoidectomy, cordotomy, and, more recently, endoscopic anterior–posterior cricoid split (EAPCS) (Otolaryngol Head Neck Surg. 2002;126:349-355; Int J Pediatr Otorhinolaryngol. 2020;138:110325) (Figure 1).
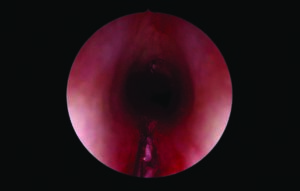
Figure 1. Zero degree Hopkins rod telescope demonstrating endoscopic anterior and posterior cricoid split. PEREIRA NM, MODI VK. LARYNGOSCOPE. DOI:10.1002/LARY.29752
While the aforementioned procedures have all been described with variable success, EAPCS has emerged as an alternative that is nondestructive and can offer a long-lasting solution to congenital BVFP while avoiding tracheostomy and minimizing the risks associated with other procedures (Int J Pediatr Otorhinolaryngol. 2020;138:110325; Laryngoscope. 2018;128:257-263). In 2017, Rutter and colleagues published a review of 19 patients who underwent EAPCS for congenital BVFP, 84% of whom were able to avoid the need for tracheostomy (Laryngoscope. 2018;128:257-263). Subsequently, Windsor and Jacobs described a series of six patients who underwent EAPCS with balloon dilation for congenital BVFP, 50% of whom were able to avoid the need for tracheostomy entirely, suggesting that EAPCS is effective in improving airway symptoms in a number of patients with this condition (Int J Pediatr Otorhinolaryngol. 2020;138:110325).