Officials say data provided by Regent will make it easier for otolaryngologists to comply with new regulations and help deliver more powerful research


Officials say data provided by Regent will make it easier for otolaryngologists to comply with new regulations and help deliver more powerful research

Close on the heels of the evidence-based medicine movement comes increasing pressure for physicians and health care institutions to develop and implement quality improvement measures that will not only improve quality of care, but also reduce medical costs and provide a way to measure performance by physicians and institutions. Integral to this process is the development of appropriate metrics by which to measure outcomes and physician performance that accurately reflect otolaryngology and its subspecialties. Two sessions at the recent 2011 American Academy of Otolaryngology–Head and Neck Surgery Annual Meeting held here Sept. 13 highlighted issues that are important for otolaryngologists striving to meet the growing demand for quality improvement.

For patients undergoing surgery, identification of known or suspected obstructive sleep apnea (OSA) is critical to avoid or minimize surgical complications that are increased in these patients, experts said here last month at SLEEP 2011, the 25th Annual Meeting of the Associated Professional Sleep Societies.
Dr. Johnson gave the presentation at COSM 2011.

Chemoradiation therapy (CRT) for head and neck cancer is overused at some centers in patients with early-stage laryngeal cancer, and more care should be taken not to overtreat patients with therapy that can have toxic effects, said invited lecturer Jonas Johnson, MD, at the Annual Meeting of the Triological Society, held here on April 29 as part of the Combined Otolaryngology Spring Meetings.

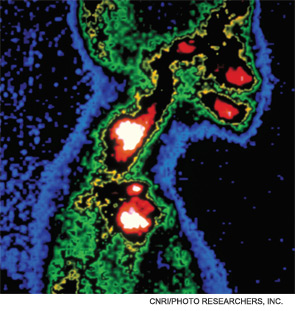
Quantitative real-time polymerase chain reaction (Q-PCR) can be a valuable tool in the operating room to determine whether head and neck cancer patients should go on to elective neck dissection, researchers said here on April 29 at the Annual Meeting of the Triological Society, held as part of the Combined Otolaryngology Spring Meetings.
Patients who had residual neck disease after treatment for a primary head and neck squamous carcinoma and then underwent neck dissection had comparable survival rates to those who had their disease resolved after their initial chemotherapy and radiation treatment, according to a retrospective analysis from researchers at the University of Louisville in Kentucky presented here Jan. 27.

The debate over soaring health care costs fails to properly acknowledge the benefits that have stemmed from improved medical technology and expanded medical knowledge, said Triological Society President Gerald Berke, MD, in an address at the society’s Combined Sections Meeting, held here on Jan. 27.
The patient-centered medical home’s star appears to be rising. Thirty-eight states are testing this model of care in some way, according to the National Academy for State Health Policy. The federal health system reform law, passed this spring, includes several provisions encouraging the concept.

Pediatric ambulatory surgery centers are fast-paced, high-volume places with many of the ingredients that can contribute to safety concerns, a patient safety expert from Children’s National Medical Center (CNMC) said at the 2010 Annual Meeting of the American Academy of Otolaryngology-Head and Neck Surgery (AAO-HNS), held here Sept. 26-29.