What is the feasibility of robotic thyroid surgery in North American patients? Background: Less invasive thyroid surgery approaches, such as video-assisted thyroidectomy, may be technically difficult and still result in a […]
Safety Net: With violence on the rise, otolaryngologists implement prevention strategies
The shooting of a doctor and two patients at Johns Hopkins Hospital in Baltimore in September sent a shudder of fear through all physicians, but for those who knew the late otolaryngologist John Kemink, MD, it was particularly saddening.
New Study Presents Education Opportunity: Nasal zinc side effects spark discussions about alternative treatments
Arecent study in Archives of Otolaryngology-Head and Neck Surgery on the potential side effects of nasal zinc therapies is the newest staging ground in the debate over how otolaryngologists can advise patients on the benefits of homeopathic treatments in the context of the common cold.
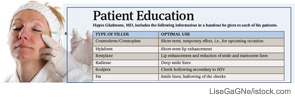
Managing Expectations: Facial plastic surgeons emphasize the limits of injectable fillers
With the availability of noninvasive procedures that use injectable fillers to do the work surgery once monopolized, more people than ever before are seeking the elixir of youth that comes now at the end of a needle rather than a knife.

A New Look at Informed Consent: Recent guidelines prompt patient-centered approach
Otolaryngologists are likely to see some changes in the way informed consent is handled at the hospitals where they perform surgery. Recent changes from the Centers for Medicare and Medicaid Services (CMS), along with Joint Commission rules, have prompted many hospitals and health systems to get more involved in what previously fell firmly in the physician’s purview.
Adverse Event Aftermath: Departments are creating programs to help physicians cope
When Rahul Shah, MD, then a pediatric otolaryngologist at Children’s Hospital in Boston, and several colleagues first undertook a survey of otolaryngologists’ reactions to adverse events in 2004, they provided a blank form for respondents to write about what had happened. In the more than 200 responses they received, Dr. Shah and his colleagues read an outpouring of emotion.

Alternative Remedies for Chronic Rhinosinusitis: Are complementary and alternative treatments harmful or advisable?
Laurie McCombs, 53, has dealt with sinus problems nearly all of her adult life. Clogged sino-nasal passages made it difficult for her to breathe at night, and the congestion caused morning pressure headaches. Over-the-counter and prescription antihistamines muted her symptoms but did not address their cause. At the age of 40, she decided to take the advice of friends who had experienced relief with acupuncture. Now McCombs follows the advice of the acupuncturist, who diagnosed her with allergies to dairy products and yeast, by limiting her intake of breads and milk products. She also continues to take loratadine and has found saline irrigation with the neti pot helpful in clearing her sinuses.
Docs Gone Bad: Your top doc just threw a tantrum. Now what?
In the more than ten years that Paul Levine, MD, FACS, has served as chair of otolaryngology and head and neck surgery at the University of Virginia in Charlottesville, he has heard his share of complaints about high-powered surgeons who are difficult to work with.

HIPAA Expansion: Ensure your practice meets the law’s new provisions
On Feb. 17, 2009, President Obama signed into law the American Recovery and Reinvestment Act of 2009 (commonly referred to as ARRA or the Stimulus Bill) which includes the Health Information Technology for Economic and Clinical Health (HITECH) Act. The HITECH Act includes significant changes to the Health Insurance Portability and Accountability Act of 1996 (HIPAA) that affect otolaryngologists and other health care providers, as well as those who process or work with health care information. Below is a summary of how these new provisions, many of which go into effect this Feb. 17, will affect your practice.

Trauma Care and the Otolaryngologist: Roles, Expectations, and Challenges
SAN DIEGO-Trauma care in the United States is on or heading toward life support. Although this may sound hyperbolic, it points to a need, seen by many otolaryngologists and other surgeons, to raise awareness of the growing gap between the numbers of people in need of trauma services and the accessibility of getting those services.
- « Previous Page
- 1
- 2
- 3
- 4
- 5
- …
- 7
- Next Page »