Physician groups representing otolaryngologists have ambitious 2011 policy and legislative agendas that include pushing for replacement of the Medicare physician payment formula and helping to shape health reform’s implementation.
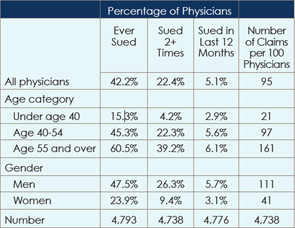
Experimental Tort Reform: States take different approaches to implement change
The health care reform law passed in March created a $50 million demonstration program to test alternatives to the current medical liability system. But reaction is mixed as to whether the new project will help fix what the physician and medical liability insurance communities view as a flawed and inefficient system.
Experts Push EHR Adoption: Expect to commit your time and finances, panelists say
The time for otolaryngologists to adopt electronic health records (EHRs) is now, practice management and information technology experts said at a session at the 2010 Annual Meeting of the American Academy of Otolaryngology-Head and Neck Surgery, held here Sept. 26-29.

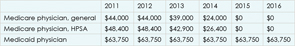
Payment Limbo: Medical societies take on SGR reform
In June, Congress gave physicians relief from the scheduled 21 percent Medicare pay cut, but only until the end of November. The payment patch, which briefly increases reimbursement by 2.2 percent, leaves doctors in limbo.

The Opt-Outs: Otolaryngologists extol the benefits of third-party independence
When describing to the curious the benefits of opting out of both Medicare and private insurance, Gerard J. Gianoli, MD, president of The Ear and Balance Institute in Baton Rouge, La., often recalls one particular example: During one 90-day global period about five years ago, after an eight-hour resection of a skull-based glomus tumor, post-operative ICU care and several days of inpatient care and the usual post-operative office visits, he received a total reimbursement of $500.
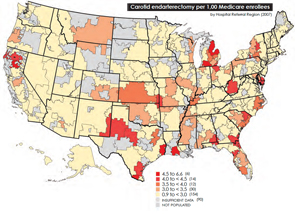
Medicare Battle Heats Up: Geographic Disparities spark look into spending variation
In the wake of this year’s landmark health care reform legislation, one of the most hotly debated topics comes courtesy of the Dartmouth Atlas of Health Care, as politicians, analysts, researchers and physicians grapple over how to resolve the contentious issue of geographical disparities in health care spending.

A New Look at Informed Consent: Recent guidelines prompt patient-centered approach
Otolaryngologists are likely to see some changes in the way informed consent is handled at the hospitals where they perform surgery. Recent changes from the Centers for Medicare and Medicaid Services (CMS), along with Joint Commission rules, have prompted many hospitals and health systems to get more involved in what previously fell firmly in the physician’s purview.
Audit Agony: Prepare yourself as insurers look to recoup funds
Hayes Wanamaker, MD, an otolaryngologist in Syracuse, N.Y., refers to the recovery audit process of insurance carriers as the proverbial camel’s nose under the tent.
A Better Way to Implement EMRs: Why one-size-fits-all won’t work
I have been a strong advocate of electronic medical records (EMRs) for almost a decade. In fact, I used the phrases “It is the silver bullet for health care reform infrastructure” and “It is the cornerstone for health care reform infrastructure” to describe EMR plans when President Obama was campaigning. However, technology, like fire, can warm your house or burn it down, cook your food or kill you. Likewise, the wrong EMR will escalate inefficiency and raise health care costs. The wrong mandates or the wrong incentives have the potential to paralyze the day-to-day practice of medicine.
Digital Dilemma: Physicians oppose EHR requirements
The federal government’s proposed rule establishing incentive payments for physicians who “meaningfully use” electronic health records (EHRs) is too onerous and would discourage physicians from participating, some otolaryngologists say.