Physician advertising can mislead patients and change the dynamic of the patient-physician relationship into one of a consumer-client relationship, said Paul A. Levine, MD, FACS, who gave the Guest of Honor presentation here on April 20 at the Triological Society annual meeting. The meeting was held as part of the Combined Otolaryngology Spring Meetings.

Tips for Avoiding a Wrongful Termination Charge
The reality for most businesses, including medical practices, is that the business owner or another employee is tasked with the uncomfortable role of terminator. If the termination is handled improperly, the former employee may lodge a complaint against you. In fact, wrongful termination charges filed with the United States Equal Employment Opportunity Commission rose last year for the seventh consecutive year.
Health Reform 101: Use this primer to navigate the changes ahead
The Patient Protection and Affordable Care Act of 2010 (ACA) is described as the most sweeping health care legislation passed in the U.S. since Medicare’s implementation in 1965. The health reform law is already changing the health care system, but the most profound modifications are yet to come. The law will affect otolaryngologists’ practices in many ways, both direct and indirect. Here are some areas of the law to consider.

ICD-10 to Bring Big Changes: Learn how to prepare for the new coding system
October 1, 2013 should be on the mind of every physician in the U.S. That is the day when a new diagnostic coding system will be instituted, the first such change since 2003. The implementation’s aftermath is predicted to be anywhere from a normal day at the office to financial Armageddon.
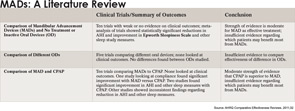
Obstructive Sleep Apnea Options
Oral appliances may work better than CPAP for some patients

Lift Off: A carefully planned retreat can take your practice to the next level
Every otolaryngology group needs a chance to evaluate its organization outside the frenetic pace of day-to-day patient care. A practice retreat provides the opportunity to assess your operations, examine your mission and conduct strategic planning in a setting where physicians are relaxed and undistracted.

Server Solution: How to choose the best server to fit your EMR needs
What’s more important, your computer’s hardware or its software? You tell me: What’s more important, your heart or your lungs? Obviously, if you’re going to function, you need both. The same is true for electronic medical record (EMR) and electronic health record (EHR) software: Your hardware is mission-critical to the success of your electronic records, and this is not the place to compromise.

Tough Situations: Residents discuss ethics-fraught cases
Residents in the general surgery program at Washington University in St. Louis, Mo., participate in monthly “pizza grand rounds,” in which they discuss ethics-fraught situations they encounter. Some of the situations are the subjects of papers published in Surgery. Here are summaries of a few of those published situations. The papers intentionally do not mention the actions ultimately taken, so that the attention remains on the principles and questions involved.

Conflicting Curriculums: Ethics education for residents inconsistent across programs

Practice Alternatives: Three otolaryngologists discuss what it’s like to work under evolving care models
Certain well-established care delivery models for otolaryngologists have long defined the specialty. But, like pharmacology, surgical techniques and treatment therapies, practice models evolve. And while traditional models continue to dominate the scope of most otolaryngology practices, the field is seeing a gradual shift to new constructs. Among them…
- « Previous Page
- 1
- …
- 6
- 7
- 8
- 9
- 10
- …
- 27
- Next Page »