 TRIO Best Practice articles are brief, structured reviews designed to provide the busy clinician with a handy outline and reference for day-to-day clinical decision making. The ENTtoday summaries below include the Background and Best Practice sections of the original article. To view the complete Laryngoscope articles free of charge, visit Laryngoscope.
TRIO Best Practice articles are brief, structured reviews designed to provide the busy clinician with a handy outline and reference for day-to-day clinical decision making. The ENTtoday summaries below include the Background and Best Practice sections of the original article. To view the complete Laryngoscope articles free of charge, visit Laryngoscope.
Explore This Issue
July 2017Background
Postirradiation otitis media with effusion (OME) due to transient edema and dysfunction of the Eustachian tube is the most common radiotherapy-associated otologic complication in patients with nasopharyngeal cancer (NPC). However, it can be seen in other head and neck cancers whose field of radiation includes the nasopharynx. Whether to insert ventilation tubes in these patients remains controversial. On one hand, ventilation tube insertion may lead to persistent otorrhea and permanent ear drum perforation; on the other hand, patients left with their serous otitis may experience
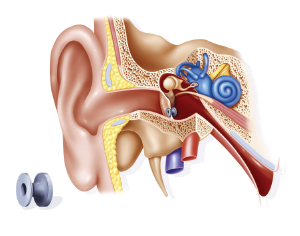
Ventilation tube set up in the ear at the level of the tympanic membrane to improve aeration of the middle ear to treat acute otitis.
© Sophie Jacopin / Science Source
hearing loss, aural fullness, tinnitus and dizziness. What is the best practice when dealing with middle ear serous effusion post radiotherapy? This review focuses on NPC, as this is the population in which radiation and ventilation tube insertion has been studied, but we feel the findings have widespread applicability in head and neck cancer.
Best Practice
A gradual approach to the management of OME postradiotherapy is recommended. The initial management should be conservative, with observation and the use of hearing aids if hearing loss is significant. If OME symptoms persist, paracentesis should be performed, with insertion of ventilation tubes (being aware of complications) reserved for patients with persistent symptoms (Laryngoscope. 2016;126:2649–2651).