Telemedicine is being used in the field of otolaryngology in a variety of ways, including real-time telemedicine, which is live, interactive, and can mimic a real-life encounter between a physician and a patient; store-and-forward approaches, in which healthcare providers collect relevant data and imaging and forward it to a consulting physician for review at a later time; and remote monitoring or diagnostics, said Garth F. Essig, Jr., MD, assistant professor of otolaryngology-head and neck surgery at The Ohio State University’s Wexner Medical Center in Columbus.
Explore This Issue
July 2017But Aaron C. Moberly, MD, assistant professor in the division of otology, neurotology, and cranial base surgery at Wexner Medical Center, said that otolaryngology has been slower to adopt telemedicine approaches compared to other fields like radiology, dermatology, and cardiology—for reasons unknown to him. Because of its reliance on more objective sources of information, such as audiograms, diagnostic imaging, and endoscopy, otolaryngology is particularly suitable for the use of telemedicine.
Benefits Abound
Telemedicine offers advantages to both otolaryngologists and their patients. First and foremost, it brings medical care to the patient so that the patient doesn’t have to travel to a medical facility. “The virtual process saves both the physician, and particularly the patient, time,” said Michael Holtel, MD, a staff surgeon at Sharp Rees Stealy Medical Group in San Diego, who cited multiple studies showing that telemedicine delivers the same or a higher level of patient satisfaction and the same quality of care (Telemed J E Health. 2016;22:209–215; Stud Health Technol Inform. 2014;196:101–106; Otolaryngol Clin North Am. 2011;44:1359–1374). The studies targeted specific visit types such as postoperative pressure equalization tube checks.
In addition to time, patients can also save money on healthcare when a telemedicine option is available. In a recent study conducted by Dr. Essig’s group, rural patients who participated in the otolaryngology telemedicine program saved close to $200 per encounter (including travels costs and lost wages) (unpublished data). Because many patients required multiple visits, this savings increased throughout the year.
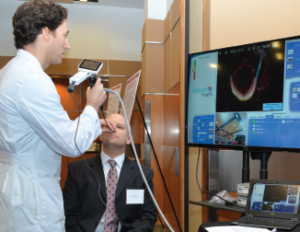
Garth Essig, MD, demonstrates a telemedicine software application to transmit real-time flexible laryngoscopy images to a distant site for telemedicine review by another practitioner.
© Courtesy of The Ohio State University Wexner Medical Center
Michael A. Keefe, MD, a facial plastic and reconstructive head and neck surgeon at Sharp Rees Stealy Medical Group, said that patients find virtual visits extremely convenient because he can use telemedicine to manage them postoperatively almost entirely, using absorbable suture and Dermabond after skin surgery and for wound care management. “It allows for closer follow-up of postoperative sites and getting the best results,” he said. “The physician can detect an issue with wound healing and the patient can send a photo if they have a concern, allowing for much more rapid and appropriate management, rather than wait[ing] for an appointment to assess the problem—which may advance the issue,” Dr. Keefe said.