Explore This Issue
November 2024Understanding the data and using evidence to support practices
Fundamental to medical decision making is the challenging task of weighing the benefits against the risks of any given treatment decision. Clinical guidelines and protocols help with this decision making, which is further informed by physician judgment, particularly when the evidence is weak or lacking.
When it comes to the use of surgical post-operative antibiotic prophylaxis, a number of guidelines on its use for prevention of surgical site infections offer recommendations skewing quite clearly toward minimizing use to avoid both adverse effects in individual patients as well as on public health with the rise of antibiotic-resistant bacteria worldwide. (National Library of Medicine. https://www.ncbi.nlm.nih.gov/books/NBK536429/)
In practice, recommendations to minimize surgical antibiotic prophylaxis are not often adhered to. Part of this may be due to long-standing protocols that don’t match the current evidence, and part may be due to issues such as patient expectations or a physician/health system erring on the side of caution to avoid any possibility of complicated and costly infections.
Maybe we should have a slightly different classification in head and neck cases because we can’t use the same logic for these cases as you can for other parts of the body, such as the abdominal or extremity surgery, where the infection risks may be higher.” — Priyesh Patel, MD
In otolaryngology, specific guidelines don’t exist to inform best practices on the use of prophylactic antibiotics for the many common surgical procedures performed. A 2011 clinical practice guideline on tonsillectomy in children recommended strongly against the routine prescription of peri-operative antibiotics in this setting (AAO-HNS. https://aao-hnsfjournals.onlinelibrary.wiley.com/doi/10.1177/0194599810389949). Until somewhat recently, no other specific guidance has been available for otolaryngologists, but more is needed. In a survey by the American Academy of Otolaryngology-Head and Neck Surgery (AAO-HNS) Infectious Disease Committee, members reported routinely prescribing pre- or post-operative antibiotics for 12 of the 17 most common procedures despite the lack of good evidence to support such use. (Otolaryngol Head Neck Surg. 2015;152:63-66.)
In 2018, Patel and colleagues filled this gap by conducting and publishing a systematic review and meta-analysis of the most current data on antibiotic prophylaxis in tonsillectomy, septoplasty/rhinoplasty, endoscopic sinus, otology, skull base, and head and neck surgeries. To date, it is the most comprehensive assessment of the evidence in otolaryngology.
Best Evidence to Date
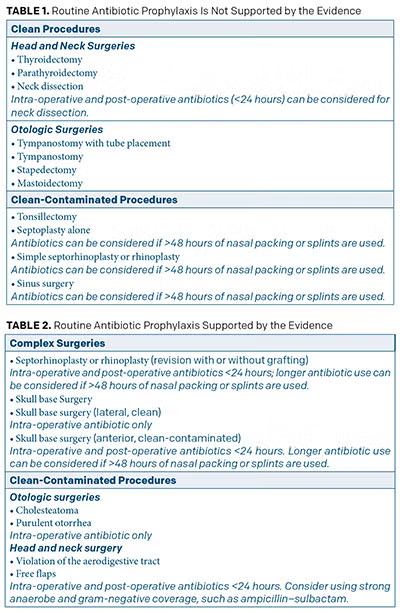 In a nutshell, the review showed that the use of routine peri-operative antibiotics for most otolaryngologic procedures is not supported by the evidence (Table 1) (Otolaryngol Head Neck Surg. 2018;158:783-800). These include clean surgeries, as well as those considered clean-contaminated.
In a nutshell, the review showed that the use of routine peri-operative antibiotics for most otolaryngologic procedures is not supported by the evidence (Table 1) (Otolaryngol Head Neck Surg. 2018;158:783-800). These include clean surgeries, as well as those considered clean-contaminated.
For surgeries for which the evidence does support prophylactic antibiotics, 24-48 hours post-operatively provides equal benefits to longer use (Table 2).
Priyesh Patel, MD, assistant professor of otolaryngology–head and neck surgery at Vanderbilt University Medical Center in Nashville, Tenn., and lead author of the study, said the findings show that even in most of the common surgical procedures performed in otolaryngology that are considered “clean-contaminated” because they require entry through the aerodigestive tract, the risk of infection is low. “I don’t know if people realize the low infection rate,” he said, citing the example of a less than 1% infection rate in sinus surgeries or septoplasty without the use of post-operative antibiotics.
He underscored the fact that for some procedures where the infection rate is still low, notably cochlear implantation, prophylactic antibiotic use is still recommended given the potentially disastrous outcomes if an infection occurs.
Dr. Patel said the decision not to use post-operative antibiotics prophylactically is often most appropriate in patients who are young and healthy and lack any complicating factors that may set them up for poor wound healing or infection. For patients at higher risk of infection, such as smokers or those with immune deficiency or diabetes, prophylactic antibiotics may be indicated even if infection rates are generally low.
Dr. Patel noted that even though most otolaryngologists use “clean-contaminated” to classify surgeries violating the aerodigestive track, he questions the real implications of the classification scheme on outcomes and infection rates. “Maybe we should have a slightly different classification in head and neck cases, because we can’t use the same logic for these cases as you can for other parts of the body, such as the abdominal or extremity surgery, where the infection risks may be higher,” he said, suggesting that a more apt classification of infection risk may help reduce the use of prophylactic antibiotics in head and neck surgery.
Other Otolaryngologists Weigh In
Philip Chen, MD, clinical professor and vice chair in the department of otolaryngology–head and neck surgery/rhinology at the University of Texas Health Science Center at San Antonio, said he thinks post-operative prophylactic antibiotics are overused in otolaryngology. “No one likes complications of surgery, and in an effort to try to minimize infection, many use antibiotics,” he said.
In the past, many patients would not feel they were adequately treated if they didn’t leave the office with some prescription, often an antibiotic. Now I am seeing more patients who are relieved I’m holding off on an antibiotic.” — Philip Chen, MD
Although he said there is a clear role for antibiotic prophylaxis for surgical fields considered “contaminated” and “dirty,” he noted situations in which its use may be more ambiguous for “clean” and “clean-contaminated” surgical fields. He cited a procedure in which an implant or foreign body is placed in the body, which may be considered a “clean” surgical site but nonetheless may increase the risk of infection. He also cited the fact that antibiotics are not regularly used in “clean-contaminated” sites such as in laryngeal or tonsil cases but are used for uninfected sinus cases despite data questioning the necessity.
“So, there is a lot to learn,” he said.
In weighing the reasonable risk of infection for a given procedure, he said otolaryngologists also need to consider both the financial and nonfinancial risks of widespread and improper use of prophylactic antibiotics. Risks he cited include patients needing higher doses of different combinations of more expensive medications to treat their disease, alterations to patients’ microbiome, potential for poorer wound healing, and risk of infections like Clostridioides difficile. Recently Dr. Chen and his colleagues published a study showing the adverse consequences, including adverse drug events, suboptimal outcomes, and increased costs, of unnecessarily treating patients who are wrongly mislabeled with a penicillin allergy with prophylactic clindamycin (Laryngoscope. 2023;133:1086-1091; Int Forum Allergy Rhinol. 2023;13:973-978).
Another consideration that may help reduce overuse, he suggests, is changing patient attitudes toward prophylactic antibiotics. “In the past, many patients would not feel they were adequately treated if they didn’t leave the office with some prescription, often an antibiotic,” he said. “Now I am seeing more patients who are relieved I’m holding off on an antibiotic.”
In the end, he hopes, “we as surgeons can be as evidence-based as possible when we prescribe these medications.”
Eric Holbrook, MD, MS, director of the division of rhinology at Massachusetts Eye and Ear and associate professor of otolaryngology–head and neck surgery at Harvard Medical School, both in Boston, who specializes in rhinology and sinus surgery, brings some clarity to the role of prophylactic antibiotics in sinus surgeries based on research he and his colleagues published in 2020 showing no benefit of prophylactic post-operative antibiotics (amoxicillin-clavulanate) over placebo on improving outcomes in patients with chronic rhinosinusitis following endoscopic sinus surgery (ESS) (Int Forum Allergy Rhinol. 2021;11:1047-1055). Although Dr. Holbrook does not routinely prescribe antibiotics after uncomplicated and non-infected surgery for his patients, he and his colleague Stacey Gray, MD, undertook the study because it remains common practice in otolaryngology to prescribe prophylactic antibiotics after ESS.
“Going into the study, we suspected that post-operative antibiotics were not needed for routine sinus surgery cases without evidence of infection,” he said, noting, “It is not totally accepted that post-operative antibiotics are not needed, so people still prescribe them.”
Dr. Holbrook said that the study’s findings disprove the assumption held by many otolaryngologists that prophylactic antibiotics are needed even if there is no evidence of infection during surgery. “I think the main reason otolaryngologists continue to prescribe prophylactic antibiotics is that it has been ingrained in their practice since training,” he said. “It’s what they have always done, and [they] believe that an infection could develop while the sinuses heal from surgery.”
Dr. Holbrook noted that one complicating factor in determining the need for prophylactic antibiotics occurs when the nose and sinuses are packed to prevent bleeding after surgery. “A lot of people are using packing after surgery, and packing can lead to patients being more prone to developing infections,” he said. Although his study did not enroll patients with packing after surgery, and therefore the findings cannot be extrapolated to these patients, he noted that there is little evidence that antibiotics are needed for patients with post-operative packing. He and his colleagues rarely use packing in their practice.
Philip E. Zapanta, MD, a general otolaryngologist at Sovah ENT & Allergy–Danville in Virginia, called it “debatable” whether or not to give antibiotics to patients with nasal packing. “When I trained in the early 2000s, we would always give antibiotics to patients who had packing for epistaxis due to the theoretical risk of toxic shock syndrome,” he said. “Now I don’t prescribe antibiotics to these patients, and patients who were packed by the ER don’t typically have prophylactic antibiotics when I see them in clinic.”
For his post-sinonasal surgery patients who have packings/splints left in place, Dr. Zapanta will give low-dose antibiotics to decrease the foul smell from packings/splints, although he said this may not be fully supported by evidence-based medicine. “For complex sinonasal surgeries, such as those that use grafts, or reconstruction or skull base surgery, I think post-op antibiotics are definitely reasonable, and the general consensus on this is clearer,” he added.
Types of Antibiotics and Duration of Use
Choosing the appropriate prophylactic antibiotic to use depends first on the surgical site and the type of bacteria that may be colonizing there. Other factors include the toxicity and potential adverse effects of the antibiotic on the patient and the antibiotic-resistant patterns found in the hospital environment in which the procedure is performed. Choosing an antibiotic that will kill bacteria (bactericidal) and not one that merely stops proliferation (bacteriostatic) is also important, as is choosing one with the potential to deeply penetrate tissue levels. These are the main criteria cited by sources in this article and detailed more broadly in a recent review by Dr. Zapanta (Medscape. https://emedicine.medscape.com/article/873812-overview).
Cefazolin (IV) and cephalexin (PO) meet most of these criteria, according to Dr. Patel, who said they are the most commonly used antibiotics in the prophylactic setting in head and neck surgeries. He noted that they are best used for gram-positive aerobic bacteria.
More controversial is the effectiveness of cefazolin for anaerobic bacteria or gram-negative bacteria. Dr. Patel said a number of studies show that clindamycin, an antibiotic with theoretically better anaerobic coverage relative to cefazolin, actually is inferior to cefazolin in several studies. “This is interesting because it is the most commonly prescribed prophylactic antibiotic in patients who are penicillin allergic,” he said, adding that it remains unclear if there is a better alternative. He said that while some studies show that antibacterial regimens with increased gram-negative coverage are associated with fewer infectious complications, many studies have failed to show benefit from improved gram-negative coverage, including the addition of aminoglycosides.
“In light of this data, the thinking is maybe you don’t need anything other than cefazolin in many situations,” he said. In cases where better gram-negative coverage may be particularly important, such as large surgical defects involving the aerodigestive track (e.g., laryngectomies or free flaps), he said that either Unasyn (IV) or Augmentin (PO) should be considered.
As to how long prophylactic antibiotics should be used, Dr. Patel said that the data generally show that long-term (defined in most studies as more than 48 to 72 hours) is not more beneficial than short-term (defined as less than 24 hours). “This is also surgery-specific,” he said. “For free flaps or very large head and neck cases, for example, data show that two days may be better than one day, but the evidence is weak.” Dr. Patel noted that it is not uncommon for physicians to prescribe antibiotics for a week or so after surgery but underscored that there is almost no data to suggest that this is beneficial. Ultimately, he said that “decisions to prescribe antibiotics are based on individual surgeon experience and patient factors” but emphasized the importance of understanding the data and using evidence to support our practices.
Mary Beth Nierengarten is a freelance medical writer based in Minnesota.