Your primary concern is the welfare of the surgeons’ patients. Secondarily, you believe this unprofessional behavior affects hospital staff morale and cohesiveness. Thirdly, these behaviors could realistically jeopardize the surgeons’ careers. The hospital chief of staff is requesting your plan for managing the complaints.
Explore This Issue
October 2014—G. Richard Holt, MD, MSE, MPH, MABE, D BE
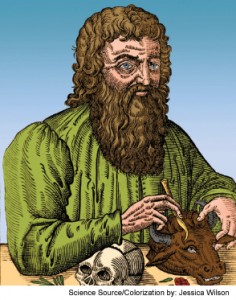
Hippocrates
The Unprofessional Physican
Discussion: This ethical dilemma can be a challenging one, with ramifications for patient care, interprofessional conflicts, medico-legal liabilities, and risks to careers. Proper physician behavior in the conduct of professional activities has been a precept (and duty) throughout the history of medicine, especially in modern times. Teaching professionalism in graduate medical education is mandated as one of the Accreditation Council for Graduate Medical Education’s Six Core Competencies. Proper modeling of professionalism by academic faculty and community preceptors is seen as foundational to the proper inculcation of desirable traits in a physician.
Medical professionalism does not have a precise definition but is a composite of appropriate behavior that encompasses a wide range of elements, including decorum, bedside manner, duties to patients (honesty, humility, respect, communication), respect of all members of the medical team, and proper adherence to the fundamentals of medical ethics in patient care (autonomy, beneficence, nonmaleficence, and social justice). Patients expect their physician(s) to exhibit proper professional behavior in the healthcare milieu while providing excellent clinical care. Patients can accept a physician’s shortcomings if their medical/surgical care is adequate; however, they should not have to settle for unprofessional behavior by their physicians.
Unprofessional behavior by physicians can include a spectrum of misconduct—a continuum of poor behavior ranging from the occasional inappropriate comment or attitude to frank, egregious conduct that jeopardizes patient well-being and safety. Increasingly, both healthcare professionals and the public are looking for evidence of “self-policing” of improper conduct by physicians and other healthcare providers, which is, of course, our profession’s fiduciary responsibility. In the absence of self-policing, regulatory agencies can, and do, step in to discipline physicians. In the scenario presented, the examples of unprofessional behavior cover a range of misconduct, from arrogance and poor communication to actual quality of care and patient safety issues. The larger the medical facility or practice, the greater the likelihood that physician leaders will have to deal with such issues. Depending on the nature of the misconduct, staff morale can be adversely affected and medical liability could be a possible concern.
Leave a Reply