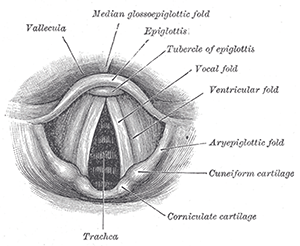
Larynx.
© Bartleby.com: Gray’s Anatomy, Plate 1204
Treating vocal fold paralysis with medialization involves a series of decisions that can sometimes be difficult to make. A panel of experts assembled at the American Academy of Otolaryngology-Head and Neck Surgery Foundation Annual Meeting to give tips to session attendees on the best approaches to surgical timing and technique, and to explain how to determine whether medialization is needed at all.
Explore This Issue
November 2016Pre-Procedure Decisions
David Francis, MD, MS, assistant professor of otolaryngology at the Vanderbilt Voice Center in Nashville, said there is often a several-month delay before someone with unilateral vocal fold paralysis actually sees a voice specialist. If a patient sees a general otolaryngologist before seeing the voice physician, it takes a median of nine months to be seen by the voice specialist. “This has significant implications for treatment planning,” he said.
The decision of whether and when to perform an injection augmentation or type I laryngoplasty requires an understanding of the physiology, along with audio-perceptual, visual-perceptual and, importantly, patient-reported factors.
When a patient comes in with vocal fold paralysis, physicians should immediately start thinking about the long-term approach. “We should be thinking about how we’re going to work up these patients and how to manage and measure outcomes systematically,” Dr. Francis said.
The question of whether imaging is needed is a matter of some controversy, he added, although there’s been a “long history” of obtaining a computerized tomography (CT) scan to assess the recurrent laryngeal nerve. “A consensus still exists that some imaging should be done to rule out mass lesions along the recurrent laryngeal nerve in most cases,” he said.
Timing from symptom onset to presentation is a key consideration when determining management. Dr. Francis said that it can take six to 12 months for the nerve to regenerate back to the laryngeal muscles it innervates after denervation injury. Determining whether and when recovery will occur is complicated; often, it is not known where the nerve is injured, how severely it is injured, and what the odds of recovery are.
He also noted that “recovery” doesn’t necessarily mean a return to normal vocal fold mobility; it is more important that symptoms improve significantly enough that a patient no longer feels that the surgery is necessary. Some patients do not experience a voice change that is severe or important enough for them to want surgery. “Even when surgeons may perceive the voice as being disordered, we must be careful not to project our biases and conceptions on these patients,” he said. Decisions about management of this condition should be patient centered and not physician centered.
Injection Laryngoplasty
Andrew McWhorter, MD, director of the Louisiana State University Voice Center in Baton Rouge, said that there is a general belief that the earlier an injection augmentation is done, the better the result. But, he said, this may not be true. Published data suggest that injection diminishes the percentage of patients eventually needing framework surgery, but it is debatable whether the timing factors into this outcome.