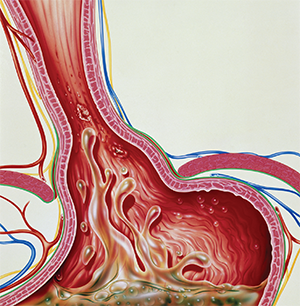
Gastroesophageal reflux.
© John Bavosi / Science Source
Despite the huge number of people who suffer from its effects, evaluation and treatment of laryngopharyngeal reflux (LPR) can vary widely, and the tools are far from perfect. Experts discussed their approach to LPR, shedding some light on many of the issues otolaryngologists face.
Explore This Issue
March 2017Moderator Seth Dailey, MD, chief of laryngology and voice surgery at the University of Wisconsin School of Medicine and Public Health in Madison, said that gastroesophageal reflux disease (GERD) affects approximately 40% of the population, with cost estimates ranging from $9 to $12 billion a year. Proton-pump inhibitors (PPIs) are the most costly prescribed medication in the U.S., he said. What’s more, the yearly cost of direct care for patients with LPR, including tests and medications, is five times what it is for patients with GERD, he said. (Am J Gastroenterol. 2013;108:905-911.)
When it comes to evaluation and treatment by otolaryngologists, he said, reflux manifests itself in many forms, and a diagnosis can be difficult to nail down. Overdiagnosis is likely common, and there can be harmful side effects from treatment.
Some of the tools otolaryngologists use have been called into question, he noted. The rigor with which the nine-question reflux symptoms index (RSI) was tested came under scrutiny in a paper published in December 2016 (Otolaryngol Head Neck Surg. 2016;155:923-935). And the reflux finding score, used to grade findings on office laryngoscopy, was found in a 2014 study to offer poor inter-rater reliability and no correlation with reflux in healthy, untreated volunteers (Laryngoscope. 2014;124:2345-51).
Dr. Dailey suggested that the field may even need to come up with a more reliable language to describe reflux. When talking about LPR, he said, “Is it disease? Is it symptoms? I’m not sure. So should we be moving toward a more common nomenclature? And where do we draw the line between what are classically described as GERD or esophageal symptoms … versus LPR symptoms?”
He and panelists also made these points as they discussed their approach to handling reflux patients.
PH Impedance Testing
Gaelyn Garrett, MD, professor of otolaryngology and senior executive medical director of the Vanderbilt Voice Center in Nashville, cautioned against otolaryngologists bringing a bias to these cases that favors a reflux diagnosis from the start. “You can’t take the next step until you evaluate other potential causes,” such as allergy or sinus, she said. “I do think reflux is a contributor in a lot of what we see, but I hate to jump directly to say, ‘How are we going to evaluate this person for their reflux symptoms?’”
She recommends reserving pH impedance testing until after testing for other upper airway inflammatory causes. “Your initial evaluation is gong to dictate that next step,” she said.
Joel Blumin, MD, chief of the division of laryngology and professional voice at the Medical College of Wisconsin in Madison, said patient preference has to be factored into the extent of testing and treatment. For example, some patients may come in only to rule out cancer, and their evaluation should be tailored with that in mind.
Peter Doble, MD, an otolaryngologist at Sawtooth Surgery Center in Twin Falls, Idaho, said he is not quick to order pH impedance testing, largely due to the rural demographics and cost-conscious nature of his patients. “I reserve testing for people who aren’t responding to any treatment modality,” he said. “I find testing to be an inadequate tool for me. … If the argument were, ‘This test is successful in making a diagnosis 85% of the time,’ then maybe we’d sell that. But if there’s more of an ‘if’ factor than that—and I think there is—it’s a very difficult sale.”
If pH impedance testing is reserved for those refractory to treatment, how is that measured? Dr. Dailey wondered. “I’m pretty sure we don’t have either a cut-off, or certainly not a uniform cut-off, as a field to be able to determine what constitutes failure,” he said. “So it seems like there’s a lot of variability, probably, if I had to guess, in terms of when to apply so-called ‘advanced testing’ and when not to.”
Interpretation
Dr. Blumin said that when performing impedance testing, symptom association to reflux events is not always easy to interpret. There are subtleties involved when trying to correlate a reflux event with a given symptom such as cough. When they do coincide, he said, “It’s nice when it happens.”
Dr. Doble said that a patient with long-time cough who takes a PPI every day might be difficult to assess. “I might stop PPIs for 30 to 45 days to see if symptoms change or worsen,” he said. If the symptoms are unchanged, he would look into other causes.
Dr. Garrett said that when considering a Nissen procedure to try to surgically correct reflux, it’s important to remember that it is generally more effective in patients who have been better responders to acid-suppression therapy and have some true GERD-type symptoms, such as heartburn.
Panelists generally agreed that pH impedance testing is a good idea after surgical procedures for reflux to quantify how well patients respond. An audience member even said that post-op findings from this test led one of the surgeons at his center to refine the technique.
Thomas Collins is a freelance medical writer based in Florida.
Take-Home Points
- Evaluation and treatment of LPR can vary widely.
- Reserve pH impedance testing until after testing for other upper airway inflammatory causes.
- A Nissen procedure is generally more effective in patients who have been better responders to acid-suppression therapy and have some true GERD-type symptoms.