A payer may prefer one documentation style over another. It is always best to query payer policy and review local documentation standards to ensure compliance. Please remember that while this example constitutes the required elements for the notation of time, documentation must also include the details of counseling, care plan revisions, and any information that is pertinent to patient care and communication with other healthcare professionals.
Explore This Issue
May 2015Family Discussions
Family discussions are a typical event involved in taking care of patients and are appropriate to count as C/CC time. Special circumstances are considered when discussions must take place without the patient present. This type of counseling time is recognized but only counts towards C/CC time if the following criteria are met and documented:
- The patient is unable or clinically incompetent to participate in discussions;
- The time is spent on the unit/floor with the family members or surrogate decision makers obtaining a medical history, reviewing the patient’s condition or prognosis, or discussing treatment or limitation(s) of treatment; and
- The conversation bears directly on the management of the patient.3
Time cannot be counted if the discussion takes place in an area outside of the patient’s unit/floor (e.g. in the physician’s office) or if the time is spent counseling the family members through their grieving process.
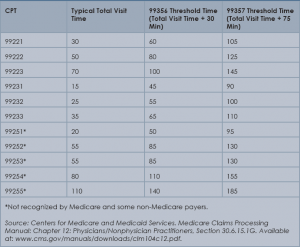
It is fairly common for the family discussion to take place later in the day, after the physician has completed morning rounds. If the earlier encounter involved C/CC, the physician would report the cumulative time spent for that service date. If the earlier encounter was a typical patient assessment incorporating the components of an evaluation (i.e., history update and physical) and management (i.e., care plan review/revision) service, the meeting time may qualify for prolonged care services.
Service Provider
Be sure to count only the physician’s time spent in C/CC. Counseling time by the nursing staff, the social worker, or the resident cannot contribute toward the physician’s total visit time. When more than one physician is involved in services throughout the day, the physicians should select a level of service representative of the combined visits and submit the appropriate code for that level under one physician’s name.4
Carol Pohlig is a billing and coding expert with the University of Pennsylvania Medical Center, Philadelphia. She is also on the faculty of the Society of Hospital Medicine’s inpatient coding course.