Dr. Leonetti typically plans a second look procedure about six to nine months post surgery. The benefits of such an approach are two-fold, he said: During the second-look surgery, “you can make sure the cholesteatoma has not recurred, and you also have a pristine environment in which to reconstruct the hearing.”
Explore This Issue
May 2010In 2006, Dr. Leonetti co-authored a review of 16 years of his experience treating pediatric cholesteatomas (Laryngoscope. 2006;116:1603-1607). The review included 106 mastoidectomies (86 acquired, 20 congenital) performed in children 16 years old and younger from 1988 to 2003. Follow-up ranged from two to 12 years, with a mean of six years.
Rates of recurrent cholesteatomas were similar in CWU and CWD patients (8 percent and 6 percent, respectively). “Good serviceable hearing,” as measured by the percent of patients with a pure-tone average greater than 25 dB, was higher in the CWU group than the CWD group (81 percent vs. 47 percent, respectively.) The researchers concluded that the CWU procedure “is an adequate surgical option for treating most acquired and congenital cholesteatomas, preventing disease recurrence and maintaining good hearing outcomes.”
Asked whether those findings hold true today, Dr. Leonetti replied, “Absolutely. We still get only about a five percent rate of patients needing repeat procedures for recurrent disease, beyond the second-look operation. And our hearing results continue to be good.”
Why do other surgeons and some published studies cite much higher rates of recurrence in children treated with CWU surgery? “I can’t really say. But one question I would ask is, ‘How much ear surgery are you doing?’ The skill, training and experience of the surgeon will all impact the final treatment outcome,” Dr. Leonetti said.
Retrograde Technique
John L. Dornhoffer, MD, director of otology/neurotology at the University of Arkansas for Medical Sciences in Little Rock, took issue with the idea that the high recurrence rates often associated with CWU surgery are surgeon-dependent to some degree.
“I’m a very experienced otologic surgeon. I’ve been trained by some of the top people in the field, and I’ve done hundreds of canal-wall-ups,” Dr. Dornhoffer said. “After seeing way too many patients who needed repeated surgeries after leaving the canal wall up, I knew there had to be a better way.”
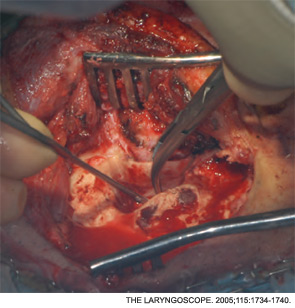
Dr. Dornhoffer eventually adopted a hybrid technique in which the upper canal wall is taken down temporarily to gain maximum exposure in the epitympanum, the cholesteatoma is removed in a retrograde approach for better visualization, and the canal defect is reconstructed using autologous cartilage from the cymba area of the conchal bowl.
Leave a Reply