Comment: Two studies highlight that cognitive impairment is common and can impact quality of life in survivors of head and neck cancers. This should impact our counseling of patients and caregivers in terms of what to expect and what is “normal.” This is also a potential productive avenue of future research in terms of elucidating methods to reduce the neurocognitive morbidity of cancer treatment. —Jennifer Villwock, MD
How is neurocognitive function impacted after definitive radiation therapy for head and neck cancer (HNC)?
Bottom line
Head and neck cancer survivors have neurocognitive sequelae up to two years after definitive chemoradiotherapy or radiation treatment.
Background: Neurocognitive deficits (NCD) have been observed in noncentral nervous system cancers, yet short- and long-term neurocognitive data on patients treated for HNC are lacking.
Study design: Prospective, longitudinal study
Study setting: Princess Margaret Cancer Centre, Toronto, Canada.
Synopsis: Neurocognitive function and self-reported symptoms were assessed in 80 patients with histologically proven HNC requiring definitive chemoradiotherapy or radiotherapy and in 40 healthy controls four times (at baseline, and at six, 12, and 24 months after baseline) prior to commencing treatment. Neurocognitive test scores were converted to age-corrected z scores (mean, 0; standard deviation, 1) and reported as mean scores, standardized regression-based scores, and frequencies of impairments in intellectual capacity, concentration, memory, executive function, processing speed, and motor dexterity. Multivariable analysis was used to identify factors associated with NCD two years after treatment.
Eighty patients and 40 healthy controls were enrolled in the study. Analyses revealed significant differences between patient and control mean performance in some domains, with patient deficits increasing over time: intellectual capacity (Cohen d, effect sizes of -0.46, -0.51, and -0.70 for time points 6, 12, and 24 months, respectively); concentration/short-term attention span (-0.19, -0.38, -0.54); verbal memory (-0.16, -0.38, -0.53); executive function (-0.14, -0.34, -0.43), and global cognitive function composite (-0.38, -0.75, -1.06). There was an increased rate of impaired global neurocognitive functioning among patients (38%) at 24 months compared with the control group (0%). Neurocognitive deficits were not associated with baseline cytokines.
Citation: Zer A, Pond GR, Razak ARA. Association of neurocognitive deficits with radiotherapy or chemoradiotherapy for patients with head and neck cancer. JAMA Otolaryngol Head Neck Surg. 2018;144:71–79.
What is the association between cognitive functioning and QoL in patients prior to treatment for HNC?
Bottom line
Cognitive impairment is common in patients with HNC and is associated with QoL and psychosocial variables. Together with previous research indicating that cognitive function and QoL can influence treatment adherence and outcomes, the results argue for the incorporation of cognitive screening and QoL assessment as part of pretreatment assessment for patients.
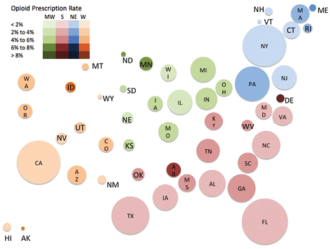
Regional variation in opioid prescribing patterns among otolaryngologists. Area of each circle is proportional to the number of total prescriptions to Medicare Part D beneficiaries (all medications), whereas the color intensity represents the proportion of prescriptions that are for opioids (key shown at inset). Southern (S) states are represented by red, Northeastern (NE) states are represented by blue, Midwestern (MW) states are represented by green, and Western (W) states are represented by orange.
Credit: © 2018 The American Laryngological, Rhinological and Otological Society, Inc.
Background: There is a dearth of research examining the associations between cognitive function and QoL in patients with HNC, despite much research examining QoL and some research examining cognitive function in this population.
Study design: Case series.
Study setting: Henry Ford Health System, Detroit.
Synopsis: Investigators collected data related to cognitive function, QoL, and psychosocial variables from 83 patients with a diagnosis of HNC between August 2015 and December 2016 who had also undergone pretreatment assessment with a clinical health psychologist and a speech and language pathologist. At pretreatment assessment, the Montreal Cognitive Assessment and Functional Assessment of Cancer Therapy–Head & Neck, version 4, were administered along with a semistructured interview to gather data on psychiatric symptoms, social support, and substance use. Patient demographic, clinical, and psychosocial variables were extracted via medical record review.
Of the 83 patients (64 [77%] male; mean age, 59.54 years), cognitive impairment was identified in 55% (n = 46) at pretreatment. The number of depressive symptoms (mean, 2.43 symptoms) was associated with impairments in delayed recall (r = −0.28) and all domains of QoL. Cognitive impairment in delayed recall was associated with lower QoL in both overall QoL and the domains of emotional and functional well-being. Current benzodiazepine use, history of heavy alcohol use, and current and past tobacco use were also associated with lower QoL in specific domains.
Citation: Williams AM, Lindholm J, Cook D, et al. Association between cognitive function and quality of life in patients with head and neck cancer. JAMA Otolaryngol Head Neck Surg.