INTRODUCTION
Subglottic stenosis is a severe and, when progressive, life-threatening condition. Throughout the past decennia, numerous surgical approaches for subglottic stenosis have been used, but the optimal procedure is yet to be determined. The surgical approaches are generally categorized as either endoscopic or open surgical repair. The most common endoscopic strategies are dilatation (through rigid or flexible dilatators or balloon dilatation), incision (cold steel or CO2 laser) followed by dilatation, or excision (cold steel or CO2 laser). All these procedures may be combined with additional stenting or (local) medical therapy (JAMA Otolaryngol Head Neck Surg. 2020;146:20-29).
Historically, for subglottic stenosis, we performed dilatation tracheoscopy using the Groningen Dilatation Tracheoscope (Ann Otol Rhinol Laryngol. 2009;118:329-335). During this dilatation tracheoscopy, ventilation of the airway distal to the stenosis is maintained through the tracheoscope. This allows for continuous dilatation of up to 10 consecutive minutes. This longer duration of dilatation is thought to be an advantage compared to the shorter duration of dilatation achieved by balloon dilatation. In conventional balloon dilatation, the airway is blocked, only allowing for intermitted dilatation for approximately 30 to 60 seconds each time and avoiding patient hypoxemia (JAMA Otolaryngol Head Neck Surg. 2017;143:500-505). A recent study in rabbits showed significantly more effect after long compared to short dilatation (Otolaryngol Head Neck Surg. 2020;163:1003-1010).
The main disadvantage of the Groningen Dilatation Tracheoscope is an increased risk of damage to the airway epithelium due to the sheer stress exerted. During balloon dilatation, the airway epithelium only endures the acting radial forces in the balloon, which has a lower risk of causing epithelial damage.
Continuous ventilation is advantageous because it allows prolonged dilation. However, a preference for balloon dilatation is argued due to the lower risk of impairing the airway epithelium.
METHOD
Between October 2020 and June 2021, seven patients with idiopathic subglottic stenosis were operated on in our institution using this new endoscopic strategy. According to the Central Committee on Research involving Human Subjects, this new treatment strategy does not require approval from an ethics committee in the Netherlands; however, all patients gave their informed consent for the procedure.
Patients were brought under general anesthesia by total intravenous anesthesia and monitored muscle relaxation. After pre-oxygenation through mask ventilation, a modified Bouchayer laryngoscope was introduced. Once the clear vision of the glottis and subglottic stenosis was achieved, the supraglottic superimposed high-frequency jet ventilation (SSHFJV) was connected. The SSHFJV uses two jet streams with different frequencies simultaneously to provide adequate oxygenation and decarboxylation. With the fast stream, the SSHFJV fires on a high frequency (usually 600/minute but up to 1,500/minute) to provide oxygenation. On the slow stream, a superimposed low frequency shifts the pressure level at the tip of the laryngoscope (some 10–20 cm H2O) up and down, typically at a frequency of 12–20/min, allowing for CO2 elimination. Oxygenation and CO2 are continuously measured transcutaneously.
Subsequently, the surgical microscope and CO2 laser were adjusted and a “Mercedes” incision of the subglottic stenosis was made by CO2 laser. This involves radial incisions to create smooth end transitions from subglottis to trachea. The stenosis was incised over its entire length at approximately 12:00, 4:00, and 8:00 (adjusted to the shape of the stenosis).
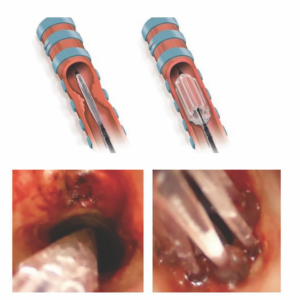
Figure 1. (A) Schematic drawing of Trachealator balloon. Left: deflated, during insertion. Right: inflated. (B) Left: Trachealator
balloon in the subglottic region and trachea before inflation. Right: inflated. The central lumen that can be used for
ventilation and oxygenation now becomes apparent.
After the Mercedes incision, the Trachealator was introduced. The Trachealator is a novel, non-occlusive balloon dilator designed for single use. Depending on its diameter, it is made up of between six and eight separate compartments. When inflated, each compartment exerts a force on the two adjacent compartments, forming a self-contained construction with an open lumen allowing for ventilation and oxygenation by the SSHFJV (Figure 1).
The diameter of the Trachealator balloon was selected according to the expected subglottic diameter for the patient based on age and sex. Each Trachealator balloon has a rated burst pressure of 14 atmospheres regardless of the size. After the Trachealator was inflated, it was held in place for 10 minutes in each patient, and, once deflated, the Trachealator was removed and the procedure was ended. Subsequently, muscle relaxation was antagonized, anesthesia was stopped, and the patients returned to spontaneous breathing.
RESULTS
During CO2 laser incision and dilation with the Trachealator, all patients (13 to 62 years of age) were adequately ventilated and oxygenated by SSHFJV. There were no perioperative or postoperative complications. All patients were examined two to four weeks and three months after surgery.
All patients reported less dyspnea/better breathing after surgery. Although subjective, all patients reported increased exercise tolerance. Two to four weeks after surgery, four out of seven patients reported glottic mucus and the need to scrape their voice. Preoperatively, our patients had a peak flow that measured 45% of their normal rates (normalized for age, gender, and height). Three months post-operation, peak-flow levels had increased to 90% of their normal rates (P < 0.05).