Explore This Issue
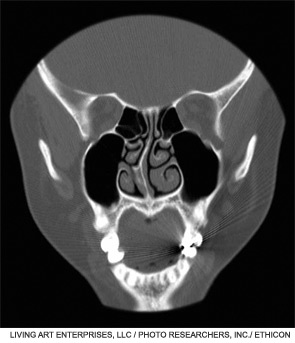
August 2011For patients who undergo septoplasty to repair a crooked septum, reconnecting pieces of cartilage and stabilizing the cartilage during the healing process is critical to achieving straight alignment of the nasal septum. Stabilizing cartilage is particularly challenging for patients who require correction of severe septal deviations or severe post-traumatic deformities that are often both functional and cosmetic.
According to Miriam Boenisch, MD, PhD, an otolaryngologist at Medicent Linz in Austria, in these cases, the cartilage needs extra support to maintain stability because the manipulations required to straighten the cartilage during a difficult septoplasty procedure also weaken the mechanical stability of the cartilage. Finding ways to provide the needed support to maintain stability through the healing phase in these more difficult and complex septoplasty procedures is critical to successful outcomes, and implants are needed, Dr. Boenisch said. Although autologous implants using bone from the posterior septum can be used, increased attention is being paid to another relatively new implant that, according to Dr. Boenisch, is more readily available than autologous implants and is easier to affix to cartilage.
Called the PDS flexible plate, the implant is made of polydioxanone, a polymer that degrades by hydrolysis and is completely resorbed by the body. It is the same polymer that has been used in PDS sutures. The implant comes in three sizes, 0.15 mm perforated, and 0.25 and 0.55 non-perforated.
"The PDS flexible plate is easily available, provides support to the operated cartilage and is resorbed by the body and thus excludes the long-term complications of artificial implants," Dr. Boenisch said.
The PDS plate has been used in Europe for many years but is still in its infancy in the U.S., having only received approval from the U.S. Food and Drug Administration (FDA) in December 2010.
European Experience
Dr. Boenisch and colleagues have been using the PDS plate since 1996 and recently reported on their long-term experience in the largest cohort of patients to date in whom the PDS plate has been used (Arch Facial Plast Surg. 2010;12(1):4-10). All 396 patients had severe septal deformities, most caused by trauma, and underwent external septoplasty followed by reconstruction of the nasal septum using the PDS plate. The technique used by Dr. Boenisch required removing the quadrangular cartilage and dividing it into its straight fragments. The trimmed fragments were then fixed to the PDS plate by polydioxanone suture material. Once affixed, the PDS plate supports the nasal dorsum until the cartilage fragments are stabilized by scar tissue.
Of the 396 patients who underwent this procedure and reconstructive process, 369 (93 percent) achieved a straight nasal septum after surgery and reported improvement in the nasal airway after surgery. In 324 (82 percent) patients, the improved nasal flow was reported as "remarkable." Overall, 18 patients (5 percent) required revision surgery to correct a redeviation or slight polly beak deformity; eight patients (2 percent) who experienced a redeviation chose not to undergo revision surgery because it caused no functional problems.
Along with effectiveness, the long-term data also show the safety of the PDS plate. Among the 396 patients treated since 1996, no complications immediately followed surgery, and no long-term complications in terms of implant rejection or septal perforation occurred.
"The clinical experience over the last 14 years shows that the PDS plate is well tolerated by the body, and even in long-term follow-up, the results of this technique are encouraging," Dr. Boenisch said.
Hesham Saleh, FRCS, a consultant rhinologist and facial plastic and ENT surgeon at Charing Cross and Royal Brompton Hospitals and Imperial College School of Medicine in London, who has used the PDS plate for about seven years in over 150 patients, said he also has had good long-term outcomes, with a 98 percent success rate in a follow-up of 100 patients who were available for analysis. Among these patients, 15 percent had minor swelling of the septum at six weeks that resulted in some continued nasal blockage, which settled down in most cases by three months, he said. Overall, 2 percent of the patients required revision surgery for residual deviation, columellar retraction and dorsal irregularity. He plans to submit these results for publication in the near future.
Dr. Saleh emphasized that the most common use of the implant is for severe septal deviations and for use as columellar struts when available cartilage is either weak or insufficient. Other applications for which he uses the implant include extension grafts, spreader grafts and endonasal septoplasty, especially in cases with caudal dislocation.
Implementation in the U.S.
Although some physicians have begun using the PDS plate based on the data coming largely from Europe, Brian Wong, MD, professor of otolaryngology-head and neck surgery and biomedical engineering at the University of California, Irvine, in Orange, Calif., emphasized that there is still a need for otolaryngologists to clarify the specific applications for which the PDS plate is valuable, particularly in cosmetic-related applications.
Current indications for use, he said, include repair of severe caudal septal deviations, in operations that involve fractured pieces of cartilage that need stabilization or reconstitution and in select applications in rhinoplasty such as attachment of caudal septal extension grafts and in the salvage of smaller cartilage specimens for use as spreader grafts and even columellar struts.
These indications highlight two main advantages of the PDS plate in specific situations. Along with providing stability to cartilage, an added value of the PDS plate is that it reduces the surgeons’ need to rely on additional cartilage grafting, said Dr. Wong, who has been involved in National Institutes of Health-funded research on cartilage for over a decade while also serving as a paid consultant for Johnson & Johnson, the company that manufactures the implant through its subsidiary Ethicon, Inc.
"I think there are definite areas where [the PDS plate] can save you an immense amount of time," Dr. Wong said. "A major value is that the PDS plate allows you to piece together cartilage segments that are fragmented to make a larger component that can be done in structural or limited load-bearing conditions. As such, you can reduce the reliance upon secondary sources of cartilage like from the ear or rib."

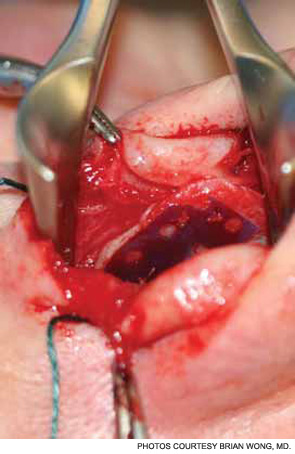
Below: A patient undergoing surgery. The specimen was used as a spreader graft in a non-load bearing application.
Dr. Wong uses mainly the 0.15 mm perforated plate because the holes facilitate some nutrient supply to the cartilage in the time interval before the plate dissolves. He is currently examining the biomechanical effects of various plate thicknesses on cartilage mechanical behavior. He said that he believes the implant may be most valuable when used to correct convex lower lateral cartilages during rhinoplasty, although he said he doesn’t have extensive experience with this particular application yet.
Dean M. Toriumi, MD, professor of facial plastic and reconstructive surgery at the University of Illinois at Chicago, said the implant can be used for correcting severe septal deformities and deviations as well as for select applications of rhinoplasty. He said he has found it to be an excellent implant to temporarily splint cartilage or cartilage grafts in cases, for example, where the cartilage is cross-hatched. He prefers the 0.25 mm plate because of its combined relative strength and because its relative thinness avoids placing too much polymer at the surgical site.
"It is excellent in applications where temporary support without adding permanent bulk is needed," he said. "Surgeons must keep in mind that it is resorbable like a PDS suture, and once it resorbs in six months, the temporary support or bulk will be gone." Dr. Toriumi has worked as a paid consultant with Ethicon, as well as Mentor Worldwide, the distributor of the device.
Minas Constantinides, MD, director of facial plastic and reconstructive surgery at New York University Medical Center in New York City and also a paid consultant for Ethicon and Mentor Worldwide, started using the PDS plate in early 2011. He said it offers a "nice" way to secure septal extension grafts and is most useful for correcting a very crooked septum. "It has given me more confidence in performing extracorporeal septoplasty to straighten these extremely challenging cases," he said. "It makes achieving a straight and strong medial crural component much easier."
The implant is also indicated for select cases of rhinoplasty, he said, including use as a carrier for dorsal or lateral onlay grafts and to create stronger spreader grafts from smaller, weaker pieces of cartilage. Ear cartilage warping can also be controlled by stenting the curved section with the plate, he said.
Cost
The key factor preventing a more widespread use of this implant among otolaryngologists and other surgeons is its cost, according to Dr. Wong.
The current price of the PDS plate is $299.00 per sheet; it is sold in a package of three sheets for a list price of $897.00 per package. According to a spokesman for Mentor Worldwide LLC, distributor of the PDS plate, the company has reduced its original price of $449.00 per sheet ($1347.00 per package) since the launch of the implant early this year. Currently, he said, the implant is not covered by insurance.
"Cost is an issue," said Dr. Toriumi, "but, if needed, surgeons are not hesitating to use it."
Best Practices
Dr. Toriumi encourages surgeons to become educated on how and when to use the implant to avoid any complications that may occur if it is not used in appropriate situations.
Dr. Saleh proposes a general guideline for otolaryngologists and other physicians to help determine when to use the implant. "Use it as scaffolding to support reconstructed cartilage anywhere in the nose when other means are inadequate, insufficient or technically difficult," he said.
 "It is excellent in applications where temporary support without adding permanent bulk is needed." – Dean M. Toriumi, MD
"It is excellent in applications where temporary support without adding permanent bulk is needed." – Dean M. Toriumi, MDAlong with the still evolving indications for use, physicians need to be aware of situations in which the implant is contraindicated. According to Drs. Saleh and Wong, the main contraindication is in patients who have had an adverse reaction to PDS sutures previously. Dr. Wong also cautioned against using the PDS plate on both sides of a cartilage graft to avoid compromising the nutrient supply to the graft, and said not to use it without complete and robust coverage by well-perfused soft tissue to avoid exposing the implant in the nasal fossa.
Dr. Constantinides emphasized the importance of not leaving the implant exposed in the nasal fossa, such as would happen in patients with a septal mucosa that is torn bilaterally; he said having the plate exposed intranasally for many weeks would disallow the survival of any attached cartilage.
Perhaps the most essential thing to note, Dr. Toriumi said, is that the PDS plate is not a replacement for cartilage and should not, for example, be used in place of cartilage for a spreader graft or alar batten graft. ENT TODAY
