What findings do laryngologists consider significant in the diagnosis of vocal fold (VF) paresis using strobolaryngoscopy, and which clinical signs are considered most compelling?
Bottom line
Most laryngologists use strobolaryngoscopy for paresis diagnosis. Although certain clinical findings were found to be associated with diagnosis, these varied among raters, especially when determining sidedness and nerve involvement.
Explore This Issue
September 2017Background: A 2015 survey of 58 fellowship-trained laryngologists found that 89% of respondents diagnosed paresis predominantly on laryngoscopic examination, with 81% of this subset relying on stroboscopic light. Laryngoscopic and stroboscopic findings believed to have the strongest positive predictive value for paresis were VF motion anomalies (slow/sluggish VF motion: 75%; decreased adduction: 67%; and decreased abduction: 65%), and signs of VF degeneration (decreased VF tone: 61%). Determining which of these clinical signs is most compelling may help further clarify diagnosis.
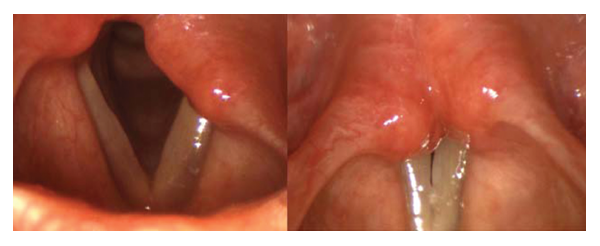
The vocal folds in abduction and during phonatory adduction on rigid strobolaryngoscopic examination. Most examiners found a left-sided (97%) paresis involving the recurrent laryngeal nerve (74%). Examiners indicated decreased VF abduction, slow/sluggish VF movement, and decreased VF adduction as the most compelling clinical findings in diagnosis.
Credit: © The American Laryngological, Rhinological and Otological Society, Inc.
Study design: Retrospective cohort study of 34 videostroboscopic examinations (24 with paresis, eight without paresis, two repeats).
Setting: Department of Otolaryngology–Head and Neck Surgery, Sean Parker Institute for the Voice, and the Department of Biostatistics and Epidemiology, Weill Cornell Medical College, New York.
Synopsis: Overall, only fair inter-rater agreement was found among raters on paresis presence or absence. Fourteen examinations (seven flexible, seven rigid) had a 70% or higher agreement that paresis was present, 11 had 70% or higher agreement on absence of paresis, and seven exams did not lean definitively toward either. The 14 exams with more than 70% agreement on paresis presence were analyzed further. Paretic-side analysis in the 14 exams showed moderate inter-rater agreement; sidedness was equally divided between left and right. Six of the 14 exams were diagnosed with recurrent laryngeal nerve (RLN) paresis (three left RLN, three right RLN) by the majority of reviewers, but all others had inconsistent diagnoses. None leaned definitively toward superior laryngeal nerve (SLN) paresis.
There were statistically significant differences in confidence levels for both side and type of paresis, between RLN and SLN paresis, and between RLN and mixed RLN/SLN paresis. The most commonly reported compelling clinical factors in the full sample were VF motion anomalies (decreased VF adduction and/or abduction, slow/sluggish VF motion (28.6%)), VF degeneration (atrophy of the hemilarynx, decreased VF tone (17.7%)), glottic insufficiency (including height difference of the VFs (15.9%)), and mucosal wave anomalies (asymmetric phase, amplitude, frequency (13.8%)). Limitations included a lack of technique information and absence of a gold standard.
Citation: Estes C, Sadoughi B, Mauer E, Christos P, Sulica L. Laryngoscopic and stroboscopic signs in the diagnosis of vocal fold paresis. Laryngoscope. 2017;127:2100–2105.