She criticized the AAO-HNS guidelines for lacking a recommendation for a postoperative sleep study in selected patients, however. "I was disappointed that the AAO-HNS guidelines did not address this, as there are published studies on several of the ‘at risk’ groups showing that while a tonsillectomy and adenoidectomy (T&A) helps with obstructive sleep apnea, it doesn’t always totally cure the OSA, especially in the children in the ‘at risk’ groups," she said.
Explore This Issue
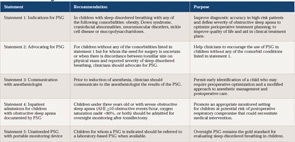
August 2011These children, she said, can forego a preoperative sleep study if they have symptoms of obstruction and sleep-disordered breathing that are confirmed by physical exam. A postoperative sleep study is more important than a preoperative sleep study to confirm to that the obstruction has been fully treated by a T&A, she said.
According to Richard M. Rosenfeld, MD, MPH, professor and chairman of otolaryngology at SUNY Downstate Medical Center in Brooklyn, N.Y., and chair of the AAO-HNS Guideline Development Task Force, the issues surrounding the postoperative use of PSG were outside the scope of the current guidelines and were addressed in the previously published 2011 guidelines on tonsillectomy (Otolaryngol Head Neck Surg. 2011;144(1 Suppl):S1-S30). Dr. Rosenfeld also pointed out that the current guidelines do emphasize that persistent sleep-disordered breathing or OSA are more common in high-risk children compared to healthy children and that the emphasis is therefore on obtaining a baseline PSG prior to surgery in high-risk children.
Dr. Shott also said the recommendation made in statement four of the AAO-HNS guidelines for postoperative observation should include more at-risk patients than those currently listed. To the current list, which includes children under three years or those with OSA and may include those with certain co-morbidities (i.e., obesity, neuromuscular or craniofacial disorders, Down syndrome, mucopolysaccharidoses and sickle cell disease), Dr. Shott would add other conditions that the AAP guidelines identified as high risk, including cardiac complications of OSA, failure to thrive, prematurity and recent respiratory infections. "The AAO-HNS guidelines discuss studies that show that it can take up to 18 hours for post operative respiratory complications to occur, and that means that respiratory complications could occur in ‘at risk’ children after they were sent home," she said.
In response to this suggestion, Dr. Rosenfeld emphasized that the comorbid conditions included in the AAO-HNS guidelines that may warrant postoperative observation are those with well-documented evidence of increased OSA severity. In addition, he said that because a PSG is recommended for all of these at-risk children, any with severe sleep apnea would be identified before surgery and admitted for observation. He acknowledged, however, that overnight observation for other children may be appropriate. "There is nothing in the document that prohibits a clinician from admitting a child with any of these conditions, and, clearly, when there are other comorbidities, such as cardiopulmonary disease, admission would be appropriate even if the [PSG} results were non-severe," he said.
Leave a Reply