Source: Seattle Children’s Hospital
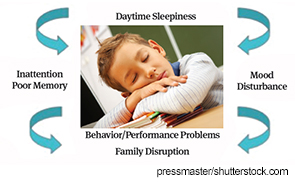
Sleep problems and disorders are common in children with chronic health conditions and, if left unrecognized and unaddressed, can have a significant negative effect on the course of the chronic illness and on overall quality of life in both the children and their families. A panel of experts at the meeting discussed the effects of sleep problems on symptom presentation and response to treatment in a variety of chronic health conditions, as well as ways to tailor sleep interventions for children based on their health conditions.
Children with chronic pain. According to Tonya M. Palermo, PhD, professor in the department of anesthesiology and pain medicine at the University of Washington and the Seattle Children’s Hospital Research Institute, up to 50% of children and adolescents with chronic pain report sleep problems, with similar sleep disturbances shown in patients with a variety of conditions that cause chronic pain, including juvenile arthritis, headache, complex regional pain syndrome, and sickle cell disease.
Insomnia is the predominant sleep problem reported in more than half of these children, she said, and is related to worse outcomes in children with chronic pain. “Youth with sleep problems/insomnia have higher levels of disability related to pain, [have] worse quality of life, and use more healthcare services,” she said, adding that research shows that sleep problems persist over time and do not remit even with improvement in pain.
She emphasized the importance of intervening to reduce sleep problems in order to interrupt the negative cycle of persistent pain and disability, as well as the need to target both sleep habits and depressive symptoms, both important predictors of chronic insomnia in this population. In particular, she said the use of behavioral strategies to treat insomnia, such as sleep restriction and stimulus control, can be very effective in youth with painful conditions.
The need for more intensive interventions, Dr. Palermo said, is highlighted by findings that cognitive behavioral pain interventions can improve pain and disability but do not appear to affect sleep.
She urged otolaryngologists to pay attention to signs of insomnia in children with chronic pain. “Particular attention should be paid to identifying difficulties with sleep onset and maintenance and making appropriate referrals for behavioral intervention for these children,” she stressed, reiterating that untreated insomnia in these children is likely to persist and have a negative impact on the chronic pain condition.
Children with asthma. Disrupted sleep in children with asthma is also related to negative outcomes, even when asthma is well controlled, said Lisa J. Melzer, PhD, assistant professor of pediatrics at National Jewish Health in Denver, who emphasized that deficient sleep can negatively affect learning, behavior, growth, and weight gain, as well as cause increased inflammation, which can lead to poorer asthma control and quality of life.
She emphasized the need for sleep interventions that address sleep hygiene, sleep duration, and insomnia symptoms, and said sleep issues in these children are treatable if identified. To that end, she encouraged screening in children with asthma for sleep problems that may be due to physiological (e.g., obstructive sleep apnea) and behavioral (e.g., insomnia) reasons, while acknowledging the challenge of screening.
“While screening for insomnia or other behavioral sleep issues would be ideal, it is unlikely to happen due to physician time constraints,” she said. “However, at the very least, otolaryngologists should be asking whether the child snores and following up as recommended by the American Academy of Pediatrics (AAP) clinical guidelines for the evaluation and treatment of sleep apnea in pediatric populations.” The AAP clinical guidelines are available at http://pediatrics.aappublications.org/content/130/3/576.
—Tonya M. Palermo, PhD
Children with cancer. Daytime fatigue and excessive daytime sleepiness are the two most important issues related to sleep disturbances in children with cancer, according to Valerie Crabtree, PhD, director of clinical services and training in the department of psychology at St. Jude Children’s Research Hospital in Memphis, Tenn.
This is particularly true for children with craniopharyngioma, who show excessive daytime sleepiness after surgery and before photon therapy, and is significantly related to lower verbal comprehension and processing speed. She emphasized that this excessive daytime sleepiness also extends into the survivorship period.
Children with other types of brain tumors also have high levels of sleepiness, particularly when they reach adolescence, she said.
The importance of recognizing and clinically managing the excessive sleepiness in these children is highlighted by the risk for negative effects of brain tumors and tumor treatment on cognition over time. “Many children who are treated for brain tumors are at risk for cognitive late effects, in which, over time, they may begin to show difficulties with processing speed, working memory, attention, and other aspects of their cognitive abilities,” she said.
One critical area Dr. Crabtree emphasized in identifying sleep issues in children with cancer is educating parents on the need to look for this in their children. She said parents often do not recognize the level of sleepiness in their children and therefore do not seek treatment.
Dr. Crabtree highlighted the need for otolaryngologists to query children with cancer as well as survivors of pediatric cancer about their level of alertness. Children found to be excessively sleepy should be managed clinically to improve daytime alertness.
She also said current research is looking at rates of sleep-disordered breathing in children with craniopharyngioma over time, because it is known that these children are at significant risk for hypothalamic obesity.
Mary Beth Nierengarten is a freelance medical writer based in Minnesota.
Leave a Reply