Mohs Surgery vs. Standard Excision
The only prospective randomized trial comparing Mohs surgery to standard excision for high-risk basal cell lesions found a difference in rate of recurrence that was not significant (4.4% vs. 12.2% for standard excision, p=0.100) in primary tumors, but significant in recurrent tumors (3.9% vs. 13.5%, p=0.023) (Eur J Cancer. 2014;50:3011-3020).
Explore This Issue
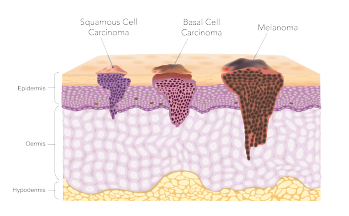
March 2020For squamous cell cancer, a meta-analysis found a difference in recurrence rate: 3% vs. 8% for primary tumors and 10% to 23% for recurrent tumors. In an analysis that included Mohs surgery, tumors 2 cm or less have been found to have a local recurrence rate of 2%, as compared with 25% for those 2 cm or greater (NCCN Guidelines Version 1. 2020. Squamous Cell Skin Cancer. Feb 18, 2020).
“How do you get your standard excision recurrence rate [to be] less?” Dr. Johnson said. “You need to look at those risk factors and treat more aggressively if you have a lot of risk factors.”
The Use of Free Flaps
© solar22 / SHUTTERSTOCK.COM
In another segment of the panel, Tamer Ghanem, MD, PhD, chief of head and neck surgery at Henry Ford Hospital in Detroit, said that free flaps can play a role in large defects when a local or pedicled flap isn’t feasible. But it’s an involved procedure that is high up on the “reconstructive ladder,” and is not one of the first considerations, he said. Because the procedure adds three to six hours to the surgery, clinicians and surgeons have to choose patients carefully.
“This is one of the most difficult parts,” Dr. Ghanem said. Physiologically, he said, “this is a fairly stressful procedure.” Patients with comorbidities might not be able to tolerate it, and the decisions might not be straightforward, he said.
Options for free flaps include the latissimus dorsi flap—the “workhorse” for large-defect scalp reconstructions, Dr. Ghanem said—as well as the radial forearm skin flap, anterolateral thigh flap, rectus abdominis muscle flap, sural flap, or a scapula or parascapula flap.
Sentinel Lymph Node Biopsies
The use of sentinel lymph node biopsy in non-melanoma skin cancers is still evolving, Dr. Ghanem said.
In one review of 53 patients who underwent a biopsy because of high-risk squamous cell carcinoma features, with adjustments for tissue processing and immunohistochemistry findings, the positivity rate was 15.1%, with a false omission rate of 7.1% (JAMA Otolaryngol Head Neck Surg. 2016;142:1171-1176).
“So, it’s not great,” he said. “We are currently using sentinel node [biopsy] for early oral cavity squamous cell cancer. And there is probably a role in skin cancer.” But compared to scanning, it’s still just the “next best thing,” he said.