What are the preoperative variables, mean operative time, morbidity, and mortality associated with reconstruction of partial glossectomy defects?
Bottom line
Free flap reconstruction of glossectomy defects involving up to half of the tongue is associated with increased morbidity and operative time when compared with nonflap reconstruction. Currently available functional outcomes data for tongue reconstruction are poor. Possible functional impairment must be weighed against the associated morbidity when deciding which defects require reconstruction, and the decision to reconstruct should not be taken lightly.
Background: The tongue remains the most common site of primary oral cavity malignant neoplasms. The type of reconstruction used for defects following ablative surgical treatment of tongue cancer is highly dependent on the extent of the resection. Tongue resections are generally classified into four groups: partial, hemi, subtotal, and total glossectomy. The degree of swallowing and speech functional impairment is dependent on the extent of tissue removed as well as the degree of functionality of residual tongue tissue. Algorithms have been established to dictate the most adequate types of reconstructions available for a given size of glossectomy defect. Over recent years, several quality of life (QOL) instruments have been adapted to study the head and neck population. Interestingly, certain studies have shown that patients undergoing reconstructions of small partial glossectomy defects may actually have worse QOL scores related to speech and swallowing than those undergoing primary closure or granulation. Furthermore, overall QOL scores of patients undergoing partial glossectomies with primary closures or granulation have been shown to be reasonably high, substantiating the argument that patients undergoing limited glossectomies should be spared the potential added morbidity of free flap reconstructions.
Study Design: Retrospective data analysis.
Synopsis: The American College of Surgeons National Surgical Quality Improvement Program database was queried for patients who had received glossectomy procedures. The study sample was split into two groups based on the lack or presence of a flap reconstruction. A total of 1,012 glossectomy patients were identified, with 805 undergoing nonflap reconstruction and 207 undergoing free flap reconstruction. Variables evaluated included wound complications, major and minor morbidity, return to the operating room, mortality, and mean operative time. Patients undergoing free flap reconstruction experienced significantly longer mean operative times (482.1 vs. 183.0 minutes), were more likely to return to the operating room, and had higher likelihood of wound complications, major morbidity, and minor morbidity. There was no difference in mortality between groups (See Figure 1).
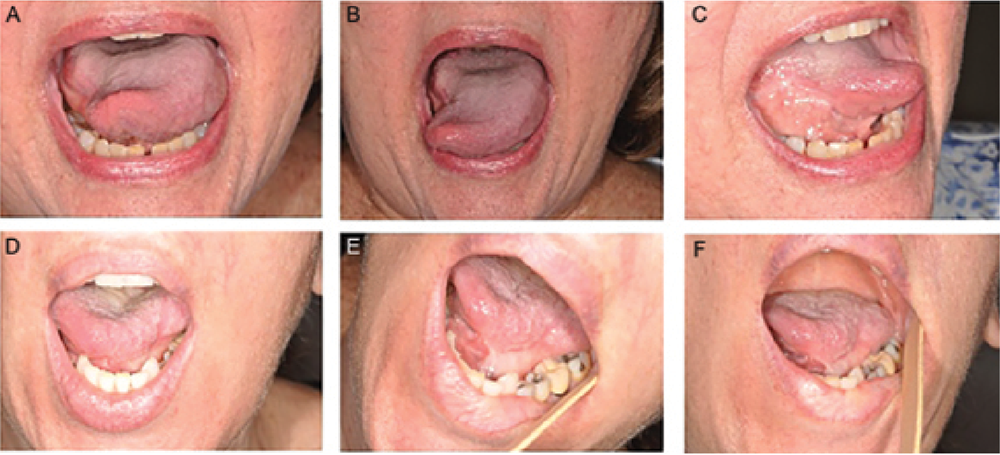
Figure 1. Granulation postoperatively. (A–C) Patient six months after partial glossectomy involving one-third of the tongue and small area of lateral floor of mouth. (D–F) Patient 15 months after partial glossectomy involving one-third of the tongue and lateral floor of mouth. Note adequate tongue protrusion with only mild tethering in both patients.
Credit: Copyright 2017 The American Laryngological, Rhinological and Otological Society, Inc.
Citation: Khan MN, Perez P, Goljo E, et al. The price of free tissue transfer after tongue reconstruction: quantifying the risks. Laryngoscope. 2017;127:1551–1557.