SAN DIEGO—Investigators from around the country presented their findings at the 120th Annual Meeting of the Triological Society, held in conjunction with the 2017 Combined Otolaryngology Spring Meetings, held here April 28–29, 2017. Here are some research highlights from the event.
Explore This Issue
June 2017Thyroid Cancer Clinical Trials in the United States
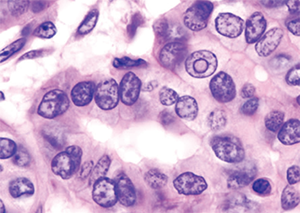
Histopatholgical image of papillary carcinoma of the thyroid gland
© Wikimedia Commons
In a retrospective analysis of U.S. clinical trials on thyroid cancer performed from 1998 through 2015, researchers found that, of the 73 trials found, 97% were drug studies. Furthermore, they found that 20% of those drug trials were focused on the kinase inhibitors sorafenib and vandetanib, with all other drugs represented in just three or fewer trials, said presenter Anand Devaiah, MD, associate professor of otolaryngology-head and neck surgery at Boston University.
The researchers also found that, among treatment type, 14% of the trials included radiation therapy and 4% involved surgery.
Dr. Devaiah said that the findings show the need for better follow through in the reporting of results, including negative results, and the need for more variety in the types of treatments that are examined in clinical trials. “We need to look at both positive and negative studies as being important to report because, without them, we’re going to end up repeating studies,” he added. “We may put patients at unnecessary risk and waste precious resources.”
Morbidity and Mortality of Oncologic Resections in Octogenarian and Older Patients with Head and Neck Cancer

© Chompoo Suriyo / SHUTTERSTOCK.COM
In a retrospective cohort study, researchers looked at patients with head and neck cancer who were at least 80 years old and who underwent surgery in non-melanoma and non-basal cell carcinoma cases.
The investigators found that 31% of patients had a serious complication
within 30 days of surgery and 11% died within 90 days of surgery. Additionally, the American Society of Anesthesiologists score, which is applied to assess physical fitness for surgery, was associated with an increased complication rate, as was an operating time of more than six hours, said Heidi L’Esperance, MD, an otolaryngology resident at Barnes-Jewish Hospital in St. Louis, who worked on the study with researchers from Washington University.
For patients aged 90 and older, severe medical comorbidities, dysphagia, and a large extent of resection were associated with an increased risk of death within 90 days.
Using these risk factors and a statistical method that clustered data, the researchers proposed a four-tier system for gauging the mortality risk of patients considered for surgery, Dr. L’Esperance said. “What we need to do is validate this in another population before it can be [put into] widespread clinical use,” she added.
Management for Octo- and Nonagenarian CI Recipients

Cochlear implant in older man.
© Life in View / Science Source
In a study on managing older patients with cochlear implants, Harold Pillsbury, MD, chair of otolaryngology–head and neck surgery at the University of North Carolina School of Medicine in Chapel Hill, said he and his team of investigators wanted to glean insights into how the care of patients older than 80 could be better managed (see “Considerations for Older Adult CI Recipients,” below).
Through a retrospective chart review, the investigators found that the most common problem with the octo- and nonagenarian patient group was loss to follow up, with 23% not returning for routine follow-up appointments. Many patients, he said, only came back if their equipment failed. Lack of follow-up was often associated with transportation challenges, he added.
Advanced age, he reminded the audience, is not a barrier to the procedure. “One of the things that goes on is, if you operate on somebody who’s over 65, you’re going to figure out that they’re going to be 90 one day and what are you going to do about it?” he said.
At his center, which has performed more than 3,400 cochlear implants for patients of all ages, patients are seen every two weeks until their performance assessment is sufficient, then every six months until stability is maintained. The center requests that older patients be accompanied by a significant member of the family “so that we can really monitor what’s going on.” Additionally, large images of the equipment and the controls also make it easier to teach patients how to use the remote control, he said.
A key to treating this population, he added, has been the use of telemedicine and the training of staff at satellite locations to make it easier for patients to be seen quickly. “This is the new way of doing it,” Dr. Pillsbury said, “and it really has made a difference for us.”
Is There a Good Side? The Role of Laterality in Facial Paralysis Severity Perceptions

Unilateral paralysis of the face.
© Dr P. Marazzi / Science Source
A randomized study has found that observers showed no preference for one side of the face over the other when viewing pictures of patients with facial paralysis, said presenter Jason Nellis, MD, a resident in otolaryngology-head and neck surgery at Johns Hopkins School of Medicine in Baltimore. The results come despite prior studies that suggested an observer preference for the left side.
In the study, naïve observers completed an online survey with photos of faces with a completely paralyzed left side or right side. For each photo of a face, a photo with a horizontal mirror image was created to control for aesthetic factors beyond the paralysis. A total of 164 observers rated the affect, attractiveness, perceived impairment, and facial paralysis severity.
While paralyzed faces were rated as significantly less attractive, as having a more negative affect, and as more impaired than normal faces, the ratings of left- and right-sided paralysis didn’t show any difference in how their attractiveness was viewed, researchers found. “This demonstrates the dominance of the paralysis effect on observer perception over the left hemiface preference,” Dr. Nellis said.
Workplace Facial Trauma On the Decline

© ndoeljindoel / shutterstock.com
A review of data on facial trauma from the U.S. Bureau of Labor Statistics
Occupational Injuries and Illnesses showed a significant decline in injuries over the period of 2004 through 2014, said Joshua Romero, MD, an otolaryngology resident at State University of New York Upstate in Syracuse.
Overall, the researchers found a total of 467,610 injuries during the 10-year time period, with a median of two days of missed work for each injury. The majority of injuries (64%) were cases of ocular trauma, but these declined from 36,680 in 2004 to 20,910 in 2014. The researchers also found that most other types of facial trauma did not significantly decline over that time, and that cases of workplace assault have significantly increased.
Overall, the incidence of workplace injuries is falling, from 10.9 injuries for every 100 workers in 1972 to 3.9 per 100 in 2014. But, researchers said that interventions targeting at-risk groups could be helpful. Young workers aged 27 to 34, who comprise 27% of the injuries, and male workers, who comprise 75% of the injuries, have the highest rate of facial injuries, and Hispanic workers are affected at a rate disproportionate to their population, Dr. Romero said.
Manual labor jobs, such as those in production and natural resources, account for an injury for approximately every 1,500 workers and are much more dangerous than office jobs, which account for an injury for every 45,000 workers, Dr. Romero said.
He added that, while incidence of facial trauma is falling and the U.S. workplace seems to be getting safer, there is room for improvement. “If targeted interventions are having an effect on ocular trauma, there could be targeted interventions available for the other subsites [of the face] that we could focus on and thus harvest some public health benefits,” he added.
Voice and Swallowing Outcomes Following Hypoglossal Nerve Stimulation for OSA
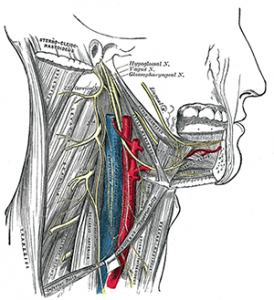
Hypoglossal nerve, cervical plexus, and their branches.
© Gray’s Anatomy (1918)
In a prospective clinical study, researchers found that hypoglossal nerve stimulation didn’t have any lasting patient-reported adverse effects on voice performance or swallowing function, said presenter Andrew Bowen, BS, a medical student at the Cleveland Clinic Lerner College of Medicine in Ohio.
Study organizers enrolled 10 patients prospectively to assess their voice and swallowing function after placement of a hypoglossal nerve stimulator for sleep apnea. Patients who were scheduled for the procedure completed a baseline Voice Handicap Index (VHI-10) and Eating Assessment Tool (EAT-10), and then completed the assessments again at one week, three months, and six months following the procedure.
The researchers found a significant spike in scores one week after the implantations, but the use of this device was not associated with any sustained, patient-reported changes in voice handicap and swallowing function. They acknowledged that no exclusion criteria or objective performance measures were used. “Future investigations are warranted,” Bowen said, “with a greater sample size, more stringent inclusion criteria, and more objective measurements.”
Thomas R. Collins is a freelance writer living in South Florida.
Considerations for Older Adult CI Recipients
- Modified follow-up schedules and additional training and materials may help with dexterity, visual, and cognitive issues.
- Follow-up is preferred to monitor performance over time and to catch potential issues early.
- Partnering with satellite clinics and/or referring PCPs, otolaryngology practices, or private practice audiologists may improve long-term follow up and prevent and identify issues early on.