SAN DIEGO—Investigators from around the country presented their findings at the 120th Annual Meeting of the Triological Society, held in conjunction with the 2017 Combined Otolaryngology Spring Meetings, held here April 28–29, 2017. Here are some research highlights from the event.
Explore This Issue
June 2017Thyroid Cancer Clinical Trials in the United States
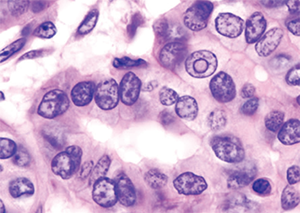
Histopatholgical image of papillary carcinoma of the thyroid gland
© Wikimedia Commons
In a retrospective analysis of U.S. clinical trials on thyroid cancer performed from 1998 through 2015, researchers found that, of the 73 trials found, 97% were drug studies. Furthermore, they found that 20% of those drug trials were focused on the kinase inhibitors sorafenib and vandetanib, with all other drugs represented in just three or fewer trials, said presenter Anand Devaiah, MD, associate professor of otolaryngology-head and neck surgery at Boston University.
The researchers also found that, among treatment type, 14% of the trials included radiation therapy and 4% involved surgery.
Dr. Devaiah said that the findings show the need for better follow through in the reporting of results, including negative results, and the need for more variety in the types of treatments that are examined in clinical trials. “We need to look at both positive and negative studies as being important to report because, without them, we’re going to end up repeating studies,” he added. “We may put patients at unnecessary risk and waste precious resources.”
Morbidity and Mortality of Oncologic Resections in Octogenarian and Older Patients with Head and Neck Cancer

© Chompoo Suriyo / SHUTTERSTOCK.COM
In a retrospective cohort study, researchers looked at patients with head and neck cancer who were at least 80 years old and who underwent surgery in non-melanoma and non-basal cell carcinoma cases.
The investigators found that 31% of patients had a serious complication
within 30 days of surgery and 11% died within 90 days of surgery. Additionally, the American Society of Anesthesiologists score, which is applied to assess physical fitness for surgery, was associated with an increased complication rate, as was an operating time of more than six hours, said Heidi L’Esperance, MD, an otolaryngology resident at Barnes-Jewish Hospital in St. Louis, who worked on the study with researchers from Washington University.
For patients aged 90 and older, severe medical comorbidities, dysphagia, and a large extent of resection were associated with an increased risk of death within 90 days.
Using these risk factors and a statistical method that clustered data, the researchers proposed a four-tier system for gauging the mortality risk of patients considered for surgery, Dr. L’Esperance said. “What we need to do is validate this in another population before it can be [put into] widespread clinical use,” she added.
Management for Octo- and Nonagenarian CI Recipients

Cochlear implant in older man.
© Life in View / Science Source