How does the reboot approach, which aims to maximally remove all sinus mucosa and allow healthy re-epithelialization from the preserved nasal mucosa, compare with classical mucosa-sparing endoscopic sinus surgery (ESS) for patients with type 2 endotype chronic rhinosinusitis with nasal polyps (CRSwNP)?
Bottom Line: The reboot approach significantly reduced nasal polyp recurrence for 30 months postoperatively compared to the current mucosa-sparing approach in patients with type 2 inflammatory CRSwNP.
Explore This Issue
June 2019Background: The percentage of CRSwNP patients with disease relapse ranges from 38% to 60% at 12 months follow-up. Peripheral, mucus, and mucosal eosinophilia have recently been discovered to affect disease severity and polyp recurrence. Difficult-to-treat CRSwNP subjects are often repeatedly exposed to various surgical managements. More extended approaches for CRSwNP have been proposed to widely access the sinuses to open them for local treatment, but removal or stripping of the mucosa was not recommended due to fear of scarring, inflammatory reactions of the denuded bone, and nonfunctional mucosa.
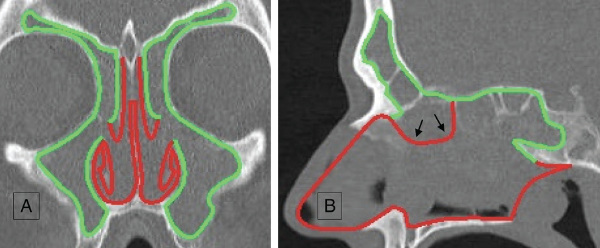
Green lines show the mucosal areas removed during the reboot surgery; red lines show the mucosal areas that are kept untouched. (A) Coronal view. Notice the untouched parts of middle turbinates kept as important suppliers for epithelial regrowth and surgical landmarks. (B) Sagittal view (black arrows point to the septal area that is removed during Draf III procedure).
© 2019 The American Laryngological, Rhinological and Otological Society, Inc.
Study design: Retrospective case-control study of 50 consecutive CRSwNP patients who underwent endoscopic sinus surgery between 2015 and 2017 (20 classical non-reboot ESS; 18 partial reboot approach; 12 complete reboot approach).
Setting: Department of Otorhinolaryngology, Ghent University, Ghent, Belgium.
Synopsis: Thirty-three of the participants had, in total, 76 previous sinus surgeries before inclusion in the study. Thirty-two of 50 patients had a history of bronchial asthma; four had aspirin-exacerbated respiratory disease. There were no significant differences in any inflammatory parameters in nasal polyp tissue or serum between groups. Patients undergoing the reboot approach, with or without the frontal sinus, had significantly reduced relapse rates compared to patients undergoing classical FESS. The time from surgery to relapse was shorter in the classical FESS group compared to the reboot group. Survival analysis showed superior results for the full reboot group concerning number and timing of recurrences, followed by the partial reboot and the classical FESS groups. Postoperative
total SNOT-22 scores were significantly lower in the combined reboot group versus the classical FESS group. In postoperative follow-up time, it took up to eight weeks for the mucosa to fully re-epithialize all sinuses. The mucosa generally looked healthy and moisturized and was of normal thickness without edema or scar formation. No complications were reported in the three study groups.
Citation: Alsharif S, Jonstam K, van Zele T, et al. Endoscopic sinus surgery for type-2 CRS wNP: an endotype-based retrospective study. Laryngoscope. 2019;129:1286–1292.