In May 2024, Tanya W. Spirtos, MD, president of the California Medical Association (CMA), sent a letter to Aliza Arjoyan, senior vice president of provider partnerships and network management for Blue Shield of California. In it, Dr. Spirtos expressed CMA members’ concerns about a recent reimbursement policy change the insurer had announced regarding evaluation and management (E/M) services billed with the Current Procedural Terminology (CPT) modifier 25. The new policy would reduce by 50% reimbursement for any non-preventive E/M service appended with modifier 25 and billed with a minor procedure code.
In her letter, Dr. Spirtos charged that Blue Shield’s proposed policy change would, in effect, penalize physicians for administering “efficient, unscheduled care,” provided during time slots that many physicians hold open in anticipation of the “20 to 30% of patients who may require same-day procedures,” as noted in the letter.
According to Erin Mellon, vice president of strategic communications for the CMA, this recent move by Blue Shield of California to reduce reimbursement on modifier 25-billed services is not unique. “The Blue Shield modifier 25 policy was just the latest in a series of attempts of payers to contain costs—often in violation of California law and industry standards—by bluntly penalizing physicians using the modifier appropriately,” Mellon said.
Such payer pushback on reimbursement for modifier 25-billed E/M services has been an ongoing challenge, said Lance A. Manning, MD, the advocacy coordinator on the board of directors for the American Academy of Otolaryngology-Head and Neck Surgery (AAO-HNS). “Problems with the 25 modifier have been cyclical over the last decade,” he said. “The AAO-HNS has successfully defended the proper use of this modifier several times during that period. Unfortunately, the private payers then bring this up several years later, and our physicians must face the same problem again.”
Separate Service
As described by the American Medical Association (AMA), modifier 25 “is used to indicate that a patient’s condition required a significant, separately identifiable E/M service above and beyond that associated with another procedure or service being reported by the same physician or other qualified health care professional on the same date. This service must be above and beyond the other service provided or beyond the usual preoperative and postoperative care associated with the procedure or service that was performed on that same date, and it must be substantiated by documentation in the patient’s record that satisfies the relevant criteria for the respective E/M service to be reported” (American Medical Association. https://www.ama-assn.org/system/files/reporting-CPT-modifier-25.pdf).
R. Peter Manes, MD, associate professor in the division of otolaryngology, department of surgery at Yale School of Medicine in New Haven, Conn., is the Relative Value Scale Update Committee (RUC) advisor for the AAO-HNS. He offers this hypothetical description of the appropriate use of modifier 25 in the otolaryngology world: “One very common complaint we see in our practice is hoarseness. At times, we are unable to get a good exam of the vocal cords using a mirror, which would be an indirect laryngoscopy. This would be a good time to perform a procedure and use a flexible scope through the nostrils and examine the vocal cords that way. In that case, we would append a 25 modifier to an E/M visit because we had to do an additional procedure beyond the scope of the E/M to adequately evaluate that patient’s particular problem.”
Currently, one-third of our office visits are appended with the 25 modifier. —Kevin Watson, chief executive officer of Raleigh Capitol Ear, Nose & Throat
To outsiders, modifier 25 payment might seem a minor issue, something that occurs infrequently with little impact on physicians or their patients. However, they would be wrong, as Kevin Watson, MHA, chief executive officer of Raleigh Capitol Ear, Nose & Throat in N.C., can attest. The practice runs six locations throughout the state, and its staff includes 14 ENTs and nine audiologists. “Currently, one-third of our office visits are appended with the 25 modifier,” he said. “It’s most commonly applied when our physicians perform nasal endoscopy and cerumen removal.”
Ultimately, modifier 25 saves time and money for physicians and patients. “Appropriate reimbursement of modifier 25 allows providers to offer necessary, resource-intensive, and potentially unplanned care to their patients without feeling the need to schedule a separate visit,” said Dr. Manning. “It is imperative that physicians are appropriately reimbursed for providing the medically necessary services and additional costs incurred from the time and care provided in these scenarios.”
Pattern of Pushback
It sounds like a cut-and-dried argument: Modifier 25 is appropriate for instances in which there is additional work performed and additional resources used for a separately identified E/M service with the same physician on the same day of the procedure. However, some payers have asserted an opposing point of view. In the instance of Blue Shield of California, for example, the insurer claims that its 50% payment reduction policy is to avoid reimbursing for the practice expense twice.
When properly applied and submitted, however, modifier 25 billing is not duplicative. Moreover, as explained in a 2023 AMA Council on Medical Service report presented at that year’s annual AMA meeting, the use of modifier 25 “indicates that documentation is available in the patient’s record to support the reported E/M service as significant and separately identifiable.”
As it stands now, private payers vary in their interpretation of modifier 25. Dr. Manning identifies three “paradigms” that represent the majority of claims:
- The carrier recognizes and pays for the proper utilization of the 25 modifier.
- The carrier does not accept the use of the modifier in any circumstance. Watson reports that at Raleigh Capitol, although the majority of government-funded and private payers reimburse for the both the visit and procedure when the 25 modifier is appended, “A significant number of these claims are initially denied, either in full or partially, requiring the practice to submit appeals, which consumes resources.”
- The carrier acknowledges appropriate use of the modifier but values the respective codes at only 50% of their normal value. An example would be the payer that automatically reduces payment for the second code to account for what it perceives to be overlap of the two codes. “These are the private payers that say, ‘We will accept the 25 modifier, but we’re only going to give you half of what you’re supposed to get,’” said Dr. Manes. “This just raises the same issue. There is no duplication of work. My colleagues and I work on valuation of these codes for not just hours, but days and weeks, to make sure we get these correct. For a private carrier to come in and say, ‘Well, no, it’s only half,’ is really an insult to the rigorous system that we must use to establish valuation. It’s very disrespectful.”
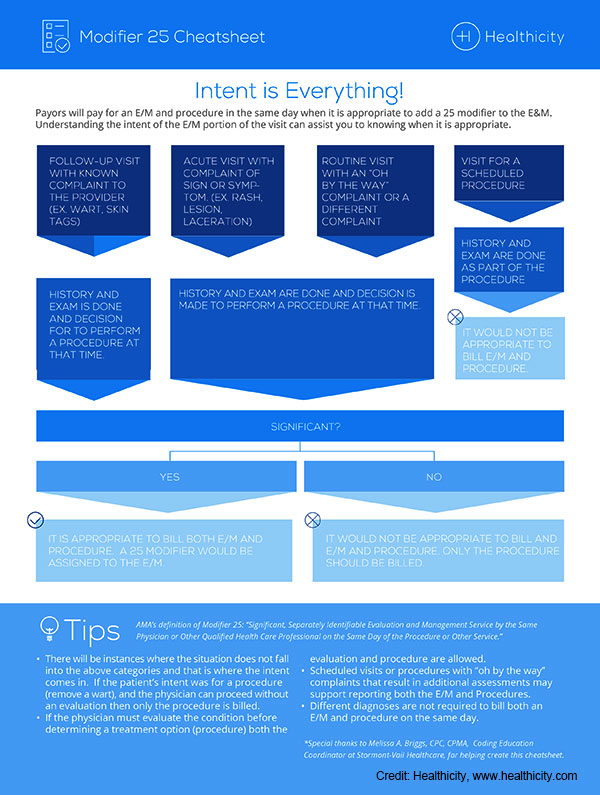
The infographic above offers a quick visual tool for determining whether a service should be appended with modifier 25.
Whether imposing a policy of non-payment or reduced payment on modifier 25 claims, failure of payers to fully reimburse has far-reaching effects, stressed Dr. Manning. “From a physician’s point of view, this results in additional services provided without resources to support them,” he said. “Over the long haul, this creates a situation in which financially compromised practices can no longer offer a full menu of services and care to their patients.”
According to the AMA report, some payers may also effectively penalize patients by “applying the deductible for one of the services or requiring the patient to come back on another date to receive the additional service.” (American Medical Association. https://www.ama-assn.org/practice-management/cpt/setting-record-straight-proper-use-modifier-25).
Like Dr. Manning, Dr. Manes views this pattern of payer pushback as cyclical. When it does come up, he finds himself going back to the basic principles of the relative value scale. “The 25 modifier is in place to appropriately value additional work and resources,” he said. “This is not trying to make something out of nothing; you are doing more, and, as a result, there should be some degree of reimbursement that reflects that. At its heart, that’s what this is about.”
Getting It Right
The American Academy of Professional Coders (AAPC), representing 22,000 members in 29 countries, has acknowledged that “… the appropriate assignment of E/M service levels and the addition of modifier 25 in the facility also have come under the Centers for Medicare and Medicaid Services’ (CMS) microscope (American Academy of Professional Coders. https://www.aapc.com/blog/24605-modifier-25-rules-cause-conflict/) .” The AAPC also points out that, even though the definition of modifier 25 is the same for facilities and physicians, “facility rules may vary from payer to payer and, in some cases, between CMS and local carriers.” Thus, given the scrutiny by payers to modifier 25 claims, there is little room for error in identifying and billing for these services.
To avoid payment denials, everyone involved in billing must be well-versed on the use of modifier 25. Watson urges practices to stay vigilant in this regard. “Physicians and advanced practice providers at Raleigh Capitol are keenly aware of the 25 modifier’s appropriate use. Nonetheless, chart reviews and audits do sometimes reveal the need to remind providers of the CPT guidance,” he said. Watson strongly recommends that all practices conduct such reviews and audits.
The AMA’s 2023 report provides the following three-question litmus test for justifying use of modifier 25:
- Did the physician perform and document the level of medical decision making or total time necessary to report a problem-oriented office or other outpatient E/M service for the complaint or problem?
- Could the work to address the complaint or problem stand alone as a reportable service?
- Did the physician perform extra work that went above and beyond the typical pre- or post-operative work associated with the procedure code?
Clinics and multilocation practices need to be especially scrupulous to ensure that everyone is up to speed. “Based on the coding knowledge of your providers, you may need to provide education,” said Watson. “Also, have staff stay informed of coding guidance and changes through organizations such as the Administrator Support Community for ENT. Lastly, remain apprised of payer policies aimed at decreasing reimbursement through modifier 25 and advocate against such efforts.”
Advocacy and Recent Action
The good news is that organized and effective action to protect modifier 25 is ongoing, and it is building on an already successful record. Dr. Manes is the former chair of the AAO-HNS physician policy work group, and he recently ended his term as the organization’s coordinator of advocacy. In both roles, he worked with the Academy’s staff and executive vice president on legislative advocacy, as well as issues concerning reimbursement, both private payer and government.
“We had great success with an effort in North Carolina that was spearheaded by one of our physician payment policy work group members, Dr. Will Harrell, and his colleagues, in that state,” reported Dr. Manes. “They discovered that a policy [against modifier 25 reimbursement] was going to be enacted, and they moved with lightning speed, engaging state medical societies and specialties societies to advocate on physicians’ behalf to this particular private payer, and they were ultimately successful in preventing enactment of the policy.”
Dr. Manning describes how the AAO-HNS closely monitors pending legislation from state to state throughout the country, including New Jersey’s S.2913, which would create a commission on insurance reimbursement. “The commission would review and approve or deny applications submitted by health insurance carriers approved to issue health benefits plans in New Jersey and which seek to reduce the payment rate for any CPT code when that code is appended with one or more modifiers,” he explained.
Physicians practicing in Massachusetts have reported incidences of health insurance carriers implementing modifier 25 policies that are negatively impacting practice costs, reported Dr. Manning. “These policies increase administrative burden across medical specialties and geographic regions, and have a potential negative effect on patients,” he said, noting that in 2023, AAO-HNS member and physician advocate Yolanda L. Troublefield, MD, JD, testified on behalf of the Massachusetts Society of Otolaryngology regarding modifier reform legislation that prohibits carriers from reducing payment when a physician uses the modifier 25 code.
What can an individual otolaryngologist do? Certainly, any carrier’s refusal to pay all or part of a modifier 25–coded fee should be appealed. Also, do not keep quiet. “Let somebody know,” advised Dr. Manes. “Remember, other specialties use 25 modifiers as well. This can help to build a groundswell of support to put pressure on carriers before they enact a policy. It’s much harder to stop a policy that has already been enacted.”
Do not forget your state-based medical organizations, whose long arms can garner the attention of private payers who rely on the state to function profitably. In the case of Blue Shield of California’s effort to reduce reimbursement by 50%, the carrier subsequently rescinded the proposed policy change, thanks to the combined push-back efforts of the CMA and numerous national and state specialty organizations. Stated Mellon, “The CMA has and will continue to push back on such policies, which would have resulted in significant, unnecessary administrative burdens and compliance costs to physician practices and would have disincentivized physicians from providing efficient care for unscheduled services.”
Linda Kossoff is a freelance medical writer based in Woodland Hills, Calif.