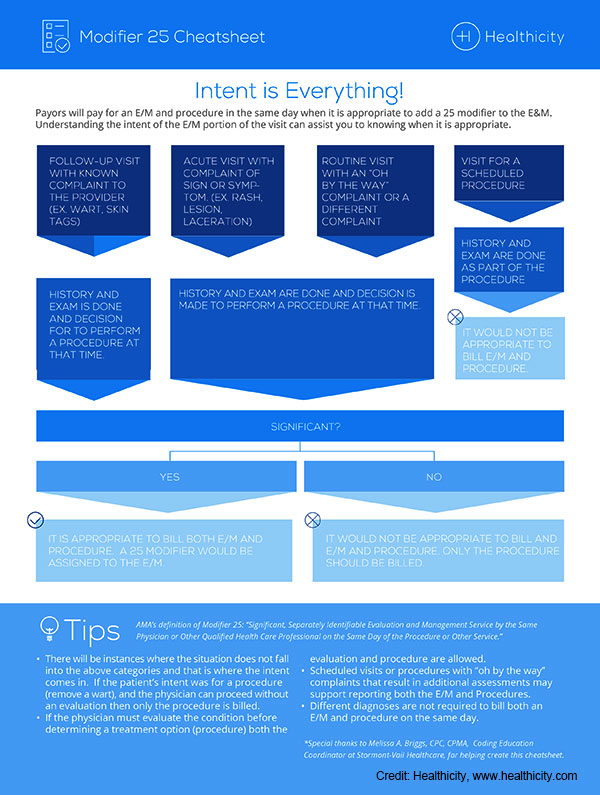
The infographic above offers a quick visual tool for determining whether a service should be appended with modifier 25.
Whether imposing a policy of non-payment or reduced payment on modifier 25 claims, failure of payers to fully reimburse has far-reaching effects, stressed Dr. Manning. “From a physician’s point of view, this results in additional services provided without resources to support them,” he said. “Over the long haul, this creates a situation in which financially compromised practices can no longer offer a full menu of services and care to their patients.”
Explore This Issue
December 2024According to the AMA report, some payers may also effectively penalize patients by “applying the deductible for one of the services or requiring the patient to come back on another date to receive the additional service.” (American Medical Association. https://www.ama-assn.org/practice-management/cpt/setting-record-straight-proper-use-modifier-25).
Like Dr. Manning, Dr. Manes views this pattern of payer pushback as cyclical. When it does come up, he finds himself going back to the basic principles of the relative value scale. “The 25 modifier is in place to appropriately value additional work and resources,” he said. “This is not trying to make something out of nothing; you are doing more, and, as a result, there should be some degree of reimbursement that reflects that. At its heart, that’s what this is about.”
Getting It Right
The American Academy of Professional Coders (AAPC), representing 22,000 members in 29 countries, has acknowledged that “… the appropriate assignment of E/M service levels and the addition of modifier 25 in the facility also have come under the Centers for Medicare and Medicaid Services’ (CMS) microscope (American Academy of Professional Coders. https://www.aapc.com/blog/24605-modifier-25-rules-cause-conflict/) .” The AAPC also points out that, even though the definition of modifier 25 is the same for facilities and physicians, “facility rules may vary from payer to payer and, in some cases, between CMS and local carriers.” Thus, given the scrutiny by payers to modifier 25 claims, there is little room for error in identifying and billing for these services.
To avoid payment denials, everyone involved in billing must be well-versed on the use of modifier 25. Watson urges practices to stay vigilant in this regard. “Physicians and advanced practice providers at Raleigh Capitol are keenly aware of the 25 modifier’s appropriate use. Nonetheless, chart reviews and audits do sometimes reveal the need to remind providers of the CPT guidance,” he said. Watson strongly recommends that all practices conduct such reviews and audits.
The AMA’s 2023 report provides the following three-question litmus test for justifying use of modifier 25:
- Did the physician perform and document the level of medical decision making or total time necessary to report a problem-oriented office or other outpatient E/M service for the complaint or problem?
- Could the work to address the complaint or problem stand alone as a reportable service?
- Did the physician perform extra work that went above and beyond the typical pre- or post-operative work associated with the procedure code?
Clinics and multilocation practices need to be especially scrupulous to ensure that everyone is up to speed. “Based on the coding knowledge of your providers, you may need to provide education,” said Watson. “Also, have staff stay informed of coding guidance and changes through organizations such as the Administrator Support Community for ENT. Lastly, remain apprised of payer policies aimed at decreasing reimbursement through modifier 25 and advocate against such efforts.”
Advocacy and Recent Action
The good news is that organized and effective action to protect modifier 25 is ongoing, and it is building on an already successful record. Dr. Manes is the former chair of the AAO-HNS physician policy work group, and he recently ended his term as the organization’s coordinator of advocacy. In both roles, he worked with the Academy’s staff and executive vice president on legislative advocacy, as well as issues concerning reimbursement, both private payer and government.
“We had great success with an effort in North Carolina that was spearheaded by one of our physician payment policy work group members, Dr. Will Harrell, and his colleagues, in that state,” reported Dr. Manes. “They discovered that a policy [against modifier 25 reimbursement] was going to be enacted, and they moved with lightning speed, engaging state medical societies and specialties societies to advocate on physicians’ behalf to this particular private payer, and they were ultimately successful in preventing enactment of the policy.”
Dr. Manning describes how the AAO-HNS closely monitors pending legislation from state to state throughout the country, including New Jersey’s S.2913, which would create a commission on insurance reimbursement. “The commission would review and approve or deny applications submitted by health insurance carriers approved to issue health benefits plans in New Jersey and which seek to reduce the payment rate for any CPT code when that code is appended with one or more modifiers,” he explained.
Physicians practicing in Massachusetts have reported incidences of health insurance carriers implementing modifier 25 policies that are negatively impacting practice costs, reported Dr. Manning. “These policies increase administrative burden across medical specialties and geographic regions, and have a potential negative effect on patients,” he said, noting that in 2023, AAO-HNS member and physician advocate Yolanda L. Troublefield, MD, JD, testified on behalf of the Massachusetts Society of Otolaryngology regarding modifier reform legislation that prohibits carriers from reducing payment when a physician uses the modifier 25 code.
What can an individual otolaryngologist do? Certainly, any carrier’s refusal to pay all or part of a modifier 25–coded fee should be appealed. Also, do not keep quiet. “Let somebody know,” advised Dr. Manes. “Remember, other specialties use 25 modifiers as well. This can help to build a groundswell of support to put pressure on carriers before they enact a policy. It’s much harder to stop a policy that has already been enacted.”
Do not forget your state-based medical organizations, whose long arms can garner the attention of private payers who rely on the state to function profitably. In the case of Blue Shield of California’s effort to reduce reimbursement by 50%, the carrier subsequently rescinded the proposed policy change, thanks to the combined push-back efforts of the CMA and numerous national and state specialty organizations. Stated Mellon, “The CMA has and will continue to push back on such policies, which would have resulted in significant, unnecessary administrative burdens and compliance costs to physician practices and would have disincentivized physicians from providing efficient care for unscheduled services.”
Linda Kossoff is a freelance medical writer based in Woodland Hills, Calif.