Applications beyond Cancer
© VectorPot / shutterstock.com
Analysis of patient genomes may also improve the treatment of many congenital anomalies, syndromes, and hearing and balance disorders caused by genetic alterations. Furthermore, with recent breakthroughs in gene-editing technology, including the use of CRISPR-Cas9 gene editing, Dr. Mandal said it may one day be possible to target these mutations in germline cells.
Explore This Issue
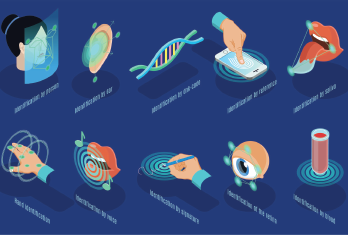
January 2019Dr. Bleier said the future of precision medicine is in developing noninvasive biosignatures from patients. “By doing this, we can sample them over time prospectively and repeatedly without causing trauma,” he said. “This will allow a physician to make a diagnosis upfront and then track how a patient’s disease evolves and responds to treatment.”
Precision medicine might also fuel efforts to identify the microbiome of the oral cavity and sinuses as a factor in chronic inflammatory conditions such as sinusitis, and evaluate its importance in explaining the individual’s susceptibility to transition from acute to chronic disease. A research group at Dr. Wang’s institution is currently studying this possibility.
Dr. Yates said that a better understanding of the genomic influences on foods, drugs, environmental effects, lifestyle choices, noise exposure, and a host of other factors may ultimately prevent problems, although this type of research is in the early stage.
Hinrich Staecker, MD, PhD, professor of otolaryngology-head and neck surgery at the University of Kansas School of Medicine in Kansas City, said treatment of sensorineural hearing loss will be significantly improved through developing biomarkers for different types of sensorineural loss. Currently, serum-based biomarkers for diverse disorders such as noise-induced hearing loss and benign paroxysmal positional vertigo are being developed. Studies identifying subtypes of Meniere’s disease are underway. “Based on these studies, we will develop pharmacotherapy and molecular therapy targeting for different types of sensorineural hearing loss,” he said.
Dr. Roehm said techniques involved in precision medicine, which couples databank searches of large amounts of patient information with NGS and other genomic evaluations of patients, could potentially identify more genes and genetic loci involved in hearing loss and aid in its treatment, as noted in a recently published study (J Genet Genomics. 2018;45(2):99-109). “Personalized patient knowledge of their genetic makeup could potentially assist in avoiding the development of hearing loss,” she said. For example, factors that predispose to ototoxic hearing loss, such as deletions in the Sod1 superoxide dismutase gene, have been identified. Physicians could inform patients with this mutation to avoid exposure to aminoglycosides due to their increased risk of hearing loss from these antibiotics.
In the future, genetic treatments specific to an identified defect will likely help to target mutations, enabling the application of highly individualized treatment approaches. Precision medicine will also likely further subclassify sensorineural hearing loss. “This could be critical in various aspects of patient management, but especially in candidacy selection for cochlear implantation,” Dr. Adunka said. “Specifically, the success or failure of hearing preservation will likely match a patient’s genetic profile obtained through precision medicine testing.”