It’s also essential to have epinephrine, steroids and oxygen readily available.
Explore This Issue
June 2013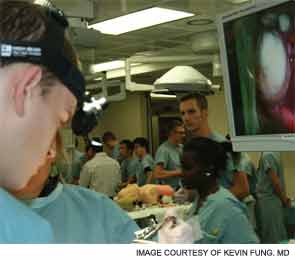
Work Together
Emergency plans should be reviewed frequently with all staff members. “We have regular meetings to remind everyone where the crash cart is, where the oxygen is and how to handle the emergency equipment,” Dr. DeSilva said. “We also talk through emergency situations. We might review what to do if someone has a heart attack in our office, for instance. We’ll go through the ACLS [advanced cardiac life support] steps so that everyone is on board and knows what to do if that situation arises.”
Dr. Zandifar’s office has an annual emergency training meeting; common emergency scenarios are also reviewed during weekly lectures with staff members.
Post-emergency debriefings are also helpful, whether the emergency was real or simulated. “When we conducted our simulation-based emergency boot camp, we found that the debriefing was one of the most important parts,” Dr. Fung said. “If a scenario took ten minutes, we’d spend 20 minutes talking about it afterward. The faculty and learners would sit around a table and talk about what went well, what didn’t go well and what could be done better next time.” A similar approach can work in an office setting.
Be sure that all staff members understand their role in emergency preparation. Beyond responding to emergency situations, a nurse or medical assistant may be responsible for monthly checks of the crash cart and emergency supplies. All staff should be up to date on emergency certifications, including basic life support and ACLS, as appropriate.
Physicians should also practice their leadership and collaboration skills. Successfully responding to an emergency involves more than clinical skills; it “also has to do with how you communicate and collaborate with other members of the health care team,” Dr. Fung said.
“Learn to be a better leader,” he said, “because you never know what kind of disaster you’re going to get in your clinic.”
Leave a Reply