Do patients with chronic sinonasal problems who initiate positive airway pressure (PAP) therapy for OSA demonstrate improved adherence with an oronasal mask versus nasal and nasal pillow interfaces?
Bottom line
The presence of nasal problems does not predict the need for an oronasal mask. Positive pressure adherence rates are higher with nasal and nasal pillow interfaces when compared with oronasal masks, even in patients with sinonasal complaints.
Background: PAP remains the standard first-line therapy for OSA, but its efficacy is limited by suboptimal adherence. Myriad patient and treatment factors affect PAP adherence, many of which are directly or indirectly related to mask interface, and poorer adherence has been previously associated with oronasal masks. Despite this correlation, there is a notion that patients with nasal obstruction may be more likely to succeed using an interface that delivers positive pressure via both the nasal and oral airways. Thus, these patients are often fit by default to oronasal masks during titration and initiation of therapy, without the opportunity to try a smaller and potentially more successful interface. Because the outcomes of PAP therapy are often determined in the first few weeks of treatment, an unfavorable initial mask choice may have adverse long-term consequences.
Study design: Retrospective analysis of medical records and polysomnography data at a tertiary-care, academic center.
Setting: University of Pittsburgh.
Synopsis: The authors reviewed 328 patients who underwent positive pressure titration between January 2012 and May 2015. Clinical data collected included baseline demographics, presence of sinonasal symptoms, smoking status, prior experience with PAP, apnea–hypopnea index (AHI), type of PAP therapy, maximum therapeutic pressure level, time to follow-up, and adherence data. The types of mask interfaces to which patients were fit were recorded and subsequently divided into three general categories: oronasal (“full face mask”), nasal, and nasal pillows.
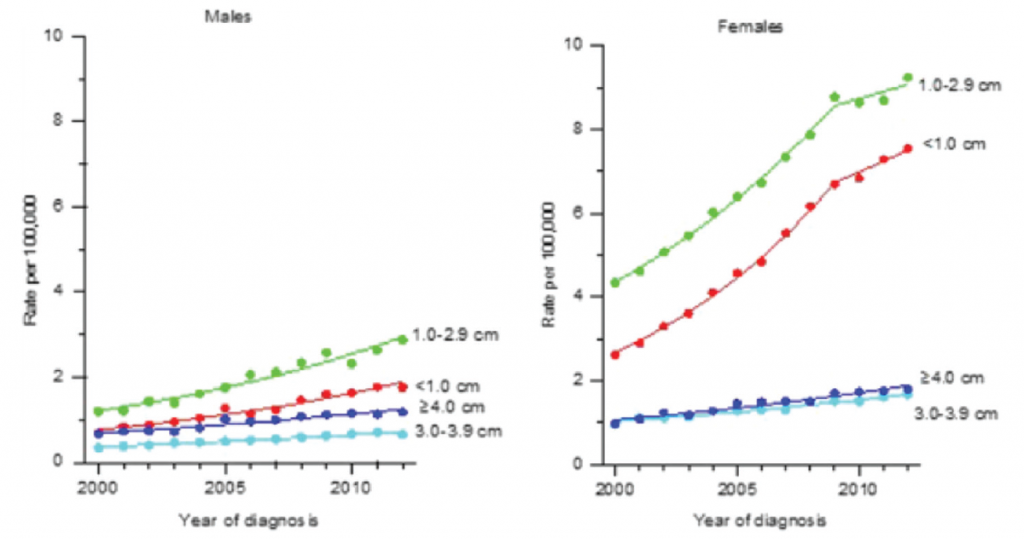
(click for larger image) Incidence rates of differentiated thyroid cancer among males and females by tumor size (SEER, 18 Registries, 2000–2012).
© The American Laryngological, Rhinological and Otological Society, Inc.
Nonadherence was defined as PAP discontinuation or usage for less than four hours per night or more than 70% of nights. The presence of sinonasal symptoms was defined as a Sinonasal Questionnaire (SNQ) score of ≥1 or explicit mention of symptomatic nasal obstruction within the sleep history if SNQ score was not available.
Follow-up adherence data were available for 218 patients (66.5%). Multivariate analysis examined whether patients with sinonasal symptoms have improved adherence with oronasal masks compared to nasal or nasal pillow interfaces. At a median follow-up of 95 days, positive pressure adherence in patients with sinonasal symptoms was highest with the nasal pillow interface. When compared with oronasal interfaces, the odds of adequate therapy adherence were more than five times greater with nasal pillow interfaces (and more than three times greater with nasal interfaces in these symptomatic patients.
Citation: Schell AE, Soose RJ. Positive airway pressure adherence and mask interface in the setting of sinonasal symptoms. Laryngoscope. 2017;127:2418–2422.