Today’s growing body of medical knowledge outpaces even the best students’ ability to retain and memorize information. According to one estimate, the entire body of medical knowledge doubles every three or four years (Trans Am Clin Climatol Assoc. 2011;122).
Explore This Issue
January 2017“Traditional methods of early medical education may no longer be relevant in the current day,” said Sonya Malekzadeh, MD, FACS, professor of otolaryngology and residency program director at Georgetown University Hospital in Washington, DC. “However, all medical students should possess a common baseline and standardized body of knowledge. Understanding anatomy, physiology, and pathology serves as a foundation for subsequent applications of this knowledge to specialized treatments and clinical outcomes.”
“There are certain things physicians should commit to memory, while other things they should be able to figure out by thinking,” said Kevin Fung, MD, associate professor in the department of otolaryngology-head and neck surgery at Western University in London, Ontario, Canada. “Patients present with problems, and our job is to solve their problems. Physicians also need training in other fundamental skills, such as communication, collaboration, team functioning, leadership, interprofessionalism, patient advocacy, health promotion, and critical appraisal.”
(click for larger image)
wikipedia
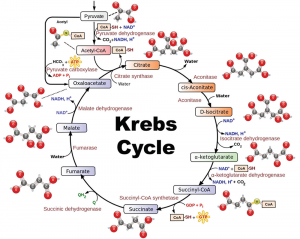
In looking at today’s educational programs, Janis Orlowski, MD, chief healthcare officer for the Association of American Medical Colleges, said that most medical schools and residency programs no longer require much memorization. “Education is more focused on how a physician can use information for problem-based learning. For instance, while physicians shouldn’t have to memorize the entire Krebs cycle, they should understand the basic functioning of a cell. Physicians can always look up something in question,” she said.
That’s indeed the preference for today’s young physicians and medical students, who seek out information in blogs and on Wikipedia, Twitter, and Facebook. “Unfortunately, the veracity of this information and the credibility of these sources is often unchecked,” said Jesus Medina, MD, an otolaryngologist at the University of Oklahoma Health Sciences Center in Oklahoma City and a member of the ENTtoday Editorial Advisory Board. “As educators, we need to direct students and trainees to credible sources of information in these media. If such sources do not exist, academicians and professional organizations should create them.”
For example, the American Head and Neck Society (AHNS) has formed the AHNS Journal Club, a committee that reviews the leading head and neck cancer-related journals and shares the most significant ones with the membership at large, via email. Dr. Medina says that the club’s format compels residents to assess reviewed articles based on their scientific merit and relevance. “Doing this month after month gives them a solid base to assess the validity of information,” he said.
Dr. Malekzadeh added, “Finding and assessing information and knowledge is the basis for lifelong learning. Ultimately, physicians must be able to identify gaps in knowledge, actively seek resources to fill needs, and assimilate and process the information to deliver quality care for best outcomes.”
Finding and assessing information and knowledge is the basis for lifelong learning. Ultimately, physicians must be able to identify gaps in knowledge, actively seek resources to fill needs, and assimilate and process the information to deliver quality care for best outcomes. —Sonya Malekzadeh, MD
Newer Learning Techniques
Another way in which education is changing is an expanding focus on team-based learning. “Evidence shows that individuals who participate in active team-based learning have superior long-term retention of information when compared to traditional passive lecture curriculum,” Dr. Malekzadeh said (Teach Learn Med. 2005;17:85-88). “Furthermore, most physicians do not practice medicine in isolation; team-based learning in education is important for developing specific skills that are essential for success in this kind of environment. Thus, faculty are developing methods to apply and integrate knowledge beyond the traditional content-based curricula, rather than course objectives such as simply memorizing a concept.”
Marita Teng, MD, residency program director and associate professor in the department of otolaryngology at Icahn School of Medicine at Mount Sinai and a member of the Head and Neck Institute at The Mount Sinai Hospital in New York City, believes educating in teams helps prepare students for the real world. “Educational research shows that it’s the most effective way for the newest generations to learn,” she said (Med Teach. 2012;34:274-278). “No one functions in a vacuum; physicians collaborate in treatment teams. It’s also practical because being a physician involves having interactions with people.”
Dr. Orlowski said her organization has advocated for interprofessional education for more than a decade. “In the past, physicians worked by themselves, but today, that is not the case; they work with pharmacists, nurses, social workers, and so forth.”
Another method, simulation-based education, provides residents with educational opportunities based on their learning needs rather than the needs of their patients, and without risk to the safety or quality of patient care (Laryngoscope. 2011;121:2114–2121). “It involves using high- or low-fidelity devices to learn techniques useful for real-life surgical situations,” said Jared J. Tompkins, MD, an otolaryngologist with Advanced ENT in Rockville, Md. “It complements traditional surgical learning situations and is not intended to replace real-life learning.”
Reverse instruction, another relatively new learning concept, requires students to review material to be learned before class. “Face-to-face classroom time can then be used to clarify or reinforce key areas or areas in which students have difficulties or questions,” Dr. Medina said. “This concept, also referred to as ‘the flipped classroom,’ may prove ideal for educating young generations because of their desire to be able to learn on demand.”
What Requires Memorization?
Despite advances in technology and learning innovations, Dr. Medina maintains that otolaryngologists should have a firm understanding of certain concepts. A sound starting point is the Comprehensive Core Curriculum assembled by the American Board of Otolaryngology, based in Houston. This curriculum, a compendium of topics, diseases, and disorders that is included in the scope of knowledge for otolaryngology-head and neck surgery, is also the foundation for board certification examinations. In addition, to comply with the requirements of the Accreditation Council for Graduate Medical Education, every residency program must have regularly scheduled didactic sessions and must provide the residents with goals and objectives for each assignment at each educational level.
The American Board of Otolaryngology and the American Academy of Otolaryngology are working together to merge their two curricula and then add educational material to improve resident education.
The bottom line: While memorizing some foundational information will likely always be necessary for physicians, learning methods will surely continue to change as the fields of medicine and technology advance.
Karen Appold is a freelance medical writer based in Pennsylvania.
IBM Watson: Translating Big Data into Big Insights
IBM Watson is a cognitive system that uses natural language processing and machine learning to translate big data from formats such as electronic medical records, images, and wearables into actionable insights. In healthcare, “Watson is serving as a trusted adviser to support physicians in making important clinical decisions,” said Kyu Rhee, MD, MPP, IBM’s chief health officer for Watson Health in Ridgefield, Conn.
On average, physicians spend approximately four to five hours a month reading medical journals. Many medical professions, however, require 29 hours per day to keep up to date. By reading all of the information in a medical chart and staying up to date with the most recent studies in journals, Watson can provide insight to physicians at the point of care, such as making them aware of a study or a piece of information in a medical chart that they didn’t recall, said Dr. Rhee.
“IBM Watson provides an opportunity for physicians to … be more predictive, proactive, and personalized as they aim to prevent bad outcomes and help promote healthy outcomes,” Dr. Rhee said.