When a resident gets a call in the middle of the night about a pediatric patient still in pain after a tonsillectomy despite taking nonsteroidal anti-inflammatory drugs (NSAIDS) or other nonopioid medications, their first inclination might be to prescribe an opioid. But experts in a session at the American Academy of Otolaryngology–Head and Neck Surgery’s (AAO-HNS) 2021 Annual Meeting said that this can be a risky way to respond.
“How do you work with your residents to not just have a knee-jerk reaction?” asked Heather M. Weinreich, MD, MPH, assistant professor of otolaryngology–head and neck surgery at the University of Illinois at Chicago.
David H. Chi, MD, chief of pediatric otolaryngology at the University of Pittsburgh School of Medicine, said he recommends a fuller discussion with the parents. “One of the first things that we’ve done with our resident team is to really emphasize the importance of counseling,” he said, “because many times parents will call in frustrated about not having pain control. The physician and the family can talk about going to the emergency room or about taking an opioid—with appropriate education about the risks.” Dr. Chi said.
Risks of Opioids
Prescribing opioids in children brings serious risk. Studies have found evidence that persistent opioid use occurs among pediatric patients when the drugs are prescribed after procedures, and that tonsillectomy and adenoidectomy are associated with prolonged opioid refills after surgery. And otolaryngologists prescribe opioids at a wide variety of rates, with a majority never prescribing them and almost 20% prescribing 30 to 60 doses per procedure (Pediatrics. 2018;141:e20172439; Pediatrics. 2015;136:e1169-e1177). A survey of more than 6,000 children found that those who used opioids legitimately before graduating from high school had a 33% increased risk of misusing them after high school (Otolaryngol Head Neck Surg. 2018;158:854-859).
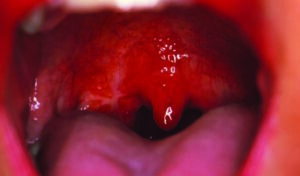
Patrick C. Walz, MD, assistant professor of otolaryngology–head and neck surgery at Nationwide Children’s Hospital in Columbus, Ohio, discussed the risk of using NSAIDS as an alternative to opioids, with some studies showing an increase in post-tonsillectomy hemorrhage (PTH) and some not.
The largest, and most recent, publication is a 2021 retrospective cohort study using data from 551,000 patients in the Pediatric Health Information System Database that found that PTH was more likely in patients who had been prescribed ibuprofen. But the researchers noted that the risk of hemorrhage was still quite small. Living in the northeastern part of the United States had a stronger association with PTH.
Overall, Dr. Walz said, the message from the evidence is that there’s a statistically significant association between PTH and the use of ibuprofen, but with a small effect size. “I would consider choosing an opioid versus ibuprofen analgesic strategy that’s specific to the patient,” he said.
Christina J. Yang, MD, attending physician in otorhinolaryngology–head and neck surgery at Montefiore Medical Center in the Bronx, N.Y., reviewed literature on other steps that can be taken to avoid opioids. In one study published in 2021, 120 patients were randomized to receive standard alternating ibuprofen and acetaminophen, or the standard care plus dexamethasone on the third day after adenotonsillectomy. The dexamethasone group had better pain scores on the third, fourth and fifth day after surgery, a decrease in pain medication use on day five, and fewer caregiver phone calls, Dr. Yang said (Otolaryngol Head Neck Surg. 2021;165:83-88).
Ninety percent of patients are not going home with an opioid now. That translates into 1,800 fewer prescriptions of opioids that are being given out per year. —Christina J. Yang, MD
Another study looked at a pediatric post-tonsillectomy protocol, with the electronic health record restricting opioids in patients under 7 years old. The practice resulted in a reduction in opioid prescriptions from 82% to 15%, with no increase in emergency room or urgent care visits, or in bleeds, Dr. Yang said (Otolaryngol Head Neck Surg. 2016;154:720-724).
But another survey of opioid use among otolaryngology patients found that 80% of them had leftover opioids after the episode of care, and that 72% of the patients kept the extra opioids that they hadn’t used (Laryngoscope. 2020;130:1913-1921).
The guidelines that address pain control in children show the need for continued work in this area, Dr. Yang said. “They have identified a need to continue in research endeavors to evaluate and compare oral postoperative pain medications so that we have as many potential strategies and alternatives at our disposal as possible.”
The panelists also described systematic steps taken to lower the amount of opioids prescribed after tonsillectomy. At Nationwide Children’s Hospital, for instance, they use an opioid consent system meant to increase education and limit abuse, and it has increased its threshold for opioid prescriptions to 4 years old.
“With these interventions we’ve been able to have a pretty significant impact. Ninety percent of patients are not going home with an opioid now. That translates into 1,800 fewer prescriptions of opioids that are being given out per year.”
Thomas R. Collins is a freelance medical writer based in Florida.