A new survey of otologists in North America, sporting an impressive 50% response rate, has shown that the use of intra-operative facial nerve monitoring (FNM) is no longer limited to tumor surgeries that have a high risk of iatrogenic facial nerve damage. Rather, nearly 90% of the respondents said they are now using FNM even during mastoid surgery, according to Jack M. Kartush, MD, a pioneer in facial nerve monitoring who conducted the survey and agreed to share the results exclusively with ENTtoday.
“This really was a surprising finding,” said Dr. Kartush, emeritus professor at the Michigan Ear Institute at Wayne State University in Detroit. “I expected most otologists to say they virtually always used facial monitoring for tumor cases, especially since monitoring was strongly advised in the 1991 NIH Consensus Conference Statement. But to see that nearly 90% of North American otologists monitor all of their mastoid operations was remarkable. It indicates that facial nerve monitoring is approaching being considered a standard of care—even in lower risk cases.”
Dr. Kartush underscored the real-world utility of the survey results. “The otologists were asked what their actual clinical practice was—not just their opinion of what they believed was a standard,” he said. He added that 94% of the respondents were fellowship trained and thus had one to two years of additional post-residency training and a high surgical volume. If such a highly specialized group uses FNM routinely, “then it follows that less experienced surgeons should have at least the same need to monitor the facial nerve,” he pointed out.
Dr. Kartush offered three caveats regarding FNM:
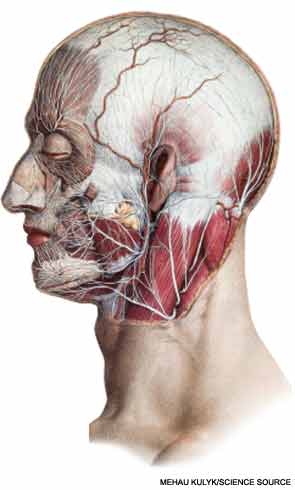
- Monitoring is not a substitute for knowledge of anatomy or surgical skills;
- Poor monitoring is worse than no monitoring; and
- Monitors fail less frequently than do “monitorists.”
In other words, no technology provides a fail-safe system for preventing human error, he said. That explains why most of the lawsuits he is asked to review now rarely make a “failure to monitor” claim, he noted. Instead, the cases typically cite “failure to monitor correctly.” That’s why proper training in FNM “is essential and drives a need for otolaryngologists to have clinical practice guidelines that not only suggest which cases should be monitored, but [also] how monitoring should be properly performed.”
Unfortunately, determining which procedures are appropriate candidates for FNM continues to be a hotly debated topic. Hoping to spur support and uptake of FNM, Dr. Kartush wrote the American Academy of Otolaryngology’s (AAO) first position statement on facial nerve monitoring two decades ago. Several years later, he followed up that effort by submitting a proposal for FNM practice guidelines to the AAO.
What the Guidelines Should Contain
Dr. Kartush reiterated that FNM guidelines need to present information not only on which cases should be monitored but also on how monitoring should be done. But those two areas of focus are not enough, he pointed out: The guidelines also must stipulate who is qualified to monitor. Here is how such a content framework could be fleshed out, he said:
- How to correctly monitor the facial nerve. Topic areas should include placing recording electrodes properly, performing a “tap test” on the electrodes, checking the electrode impedance, and using electrical stimulation routinely to assure that current is flowing and that facial muscles have not been inadvertently paralyzed by anesthesia’s use of neuromuscular blockade drugs. “These can be done like a pilot’s pre-flight checklist,” Dr. Kartush said.
- Who should perform monitoring. “If we solve the first item, we resolve the second,” he noted. “That is, if we can prove via guidelines and cited data that otolaryngologists have training and background to properly perform both the technical and interpretive aspects of FNM, that should convince insurers, neurologists, and neurophysiologists that we are well suited as a specialty to do this.”
- Which cases should be monitored. “This has been the most controversial area in the debate over FNM,” Dr. Kartush said. “But the survey is demonstrating unequivocally that FNM has now been adopted in the actual clinical practices of the great majority of otologists for tumors, tympanomastoid surgery, cochlear implants, endolymphatic sac decompressions, and transmastoid labyrinthectomy. Conversely, the survey also demonstrates that, while FNM might have a role in very low-risk procedures, most otologists do not at this time monitor every stapes or pure tympanoplasty operation.”
Reimbursement
Until such guidelines are drafted and released, another long-simmering controversy over FNM—over who should be reimbursed for the procedure—will continue. Dr. Kartush noted that Medicare, Medicaid, and many third-party insurers now refuse to pay otolaryngologists for facial nerve monitoring. In fact, their payment policies often stipulate that while other clinicians aside from the surgeon can get paid for the monitoring, the surgeon who elects to do it will not be paid.
“This is regrettable, because a surgeon trained in FNM is in an ideal situation not only to perform the technical setup of monitoring but also to properly interpret the responses,” Dr. Kartush said. “Unlike a technologist in the room or a neurologist who may perform remote monitoring from home, only the surgeon is unequivocally attuned in real-time to how their surgical maneuvers correlate to the evoked potentials.”
Dr. Kartush has argued at recent coding meetings of the American Medical Association that properly trained surgeons such as otolaryngologists are deserving of payment for FNM. The main problem, he said, is that otolaryngologists must demonstrate that intra-operative monitoring is indeed part of their core curriculum, and not just make a proclamation that monitoring is within the domain of the specialty. “Having published practice guidelines will help in that regard, further our national stance and enhance care,” he said.
As for the other specialties that are getting paid for FNM, including neurologists, audiologists, and neurophysiologists, they’ve successfully lobbied for those payments, Dr. Kartush said. “Frankly, that’s a political and advocacy challenge we need to better handle, working in concert with our professional societies.”
He acknowledged that reimbursement is a secondary concern, however, given the benefits of monitoring, as well as the relatively manageable cost of implementing FNM systems. A series of studies looked at this issue by assessing the clinical efficacy and cost benefits of FNM in middle ear and mastoid surgery. In one study, the researchers weighed quality-
adjusted life years (QALY) against the cost of care and found that a strategy employing FNM during primary and revision surgeries had the greatest effectiveness and lowest cost of all the strategies tested. Not monitoring the facial nerve had a lower QALY and the highest cost (Laryngoscope. 2003;113:1736-1745), the investigators reported. Based on the results, the authors concluded that FNM is indeed cost effective “and its routine use should be adopted to reduce the risk of iatrogenic facial nerve injury during otologic surgery.”
 Poor monitoring is worse than no monitoring. That’s why practice guidelines that outline proper setup and interpretation are critical.
Poor monitoring is worse than no monitoring. That’s why practice guidelines that outline proper setup and interpretation are critical.—Jack M. Kartush, MD
Cost Not a Consideration
Peter S. Roland, MD, chair of the department of otolaryngology-head and neck surgery at the University of Texas Southwestern Medical Center in Dallas, agreed that cost should not be a major consideration in deciding whether to use FNM during most otologic procedures. “In our case, we’ve already purchased the system; our surgeons do the monitoring, and, frankly, if there is any expense associated with it, it’s something we just absorb, because the cost of not monitoring is so high,” he said.
Those costs, Dr. Roland noted, quickly add up because of the complex interventions needed to mitigate some of the devastating effects of facial nerve injury. Those sequelae include alterations of facial appearance, exposure of the eye to vision-threatening desiccation and infection, and impairment of the oral sphincter, resulting in drooling and alterations in vocal quality, he said. “And that doesn’t even take into consideration the exorbitant cost of fighting—and in several cases, losing—malpractice cases alleging fault in cases of facial nerve injury,” he said.
Dr. Roland also offered some caveats regarding FNM. “Monitoring is not a panacea, and it does not substitute for an in-depth understanding of anatomy,” he said. In fact, “if you rely on that monitor to tell you where the facial nerve is likely located, without having a really good understanding of where it might be situated—for example, based on a structural abnormality such as dehiscence—you are heading for a world of trouble.”
“For me, going into an otologic surgery without monitoring for the facial nerve is almost like operating blind,” said Dr. Roland. “It’s a tool I certainly don’t want to be without in most cases.”
He also stressed that understanding the basics of how the various monitors work, including their proper calibration and use, is critical to success. Dr. Kartush echoed that point. “As I noted, poor monitoring is worse than no monitoring,” he said. “That’s why practice guidelines that outline proper setup and interpretation are critical.”
Survey Shows High Degree of FNM Expertise
Fortunately, the results of Dr. Kartush’s survey indicate that most otologists already follow the key steps necessary to help ensure accurate facial nerve monitoring, including assessing current flow and impedance and performing a tap test. But not all of the practitioners do so, he noted, and it is the failure to take such key steps in every operation that can allow even experienced surgeons to be lured into complacency.
“If the monitor is improperly set up and the surgeon never stimulates but only relies on the monitor to sound during mechanical trauma, they and their patient may have a heartbreaking surprise in the recovery room when an unexpected facial palsy is identified,” he said. “The facial nerve may be injured, but the alarm may not be triggered if the monitoring setup is improper.”
To help avoid such outcomes, Dr. Kartush has developed an FNM protocol that he taught to many surgeons and technologists over the decades (click here to read Dr. Kartush’s protocol). Such materials underscore the fact that “the age of practice guidelines and surgical checklists is here,” he said. “After more than a quarter century of facial nerve monitoring, it is high time to assure our specialty incorporates monitoring practice guidelines in our training programs, core curricula, and departmental programs. As in the adoption of oxygen monitoring guidelines by anesthesia, the result will benefit patient and surgeons alike.”
David Bronstein is a freelance medical writer based in New Jersey.
Leave a Reply