
Fred Minnick spent more than a year in Iraq as a U.S. Army public affairs photojournalist. He survived a near-direct hit by a rocket-propelled grenade but lost a lot of his hearing. Today, at the age of 34, Minnick struggles to hear people in crowds and is subject to near-constant ringing in his ears. His auditory issues affect both his professional and his personal life.
“You know how if someone has a stroke, they slur a lot? That’s what a lot of people sound like to me. I have a hard time understanding people on speakerphone or on convention floors. I’ll interview someone on the phone and have no idea what the heck they’re saying,” said Minnick, who is also the author of Camera Boy: An Army Journalist’s War in Iraq (Hellgate Press, 2010).
His colleagues and friends don’t always understand and appreciate his hearing difficulty, said Minnick, and that can lead to interpersonal problems. “People with hearing loss … suffer a lot of ridicule and misunderstanding,” Minnick said. “We also misunderstand people. Sometimes it sounds, to us, like someone is being aggressive, and that’s not the case at all. It’s actually a case of them trying to talk loud because they know we can’t hear.”
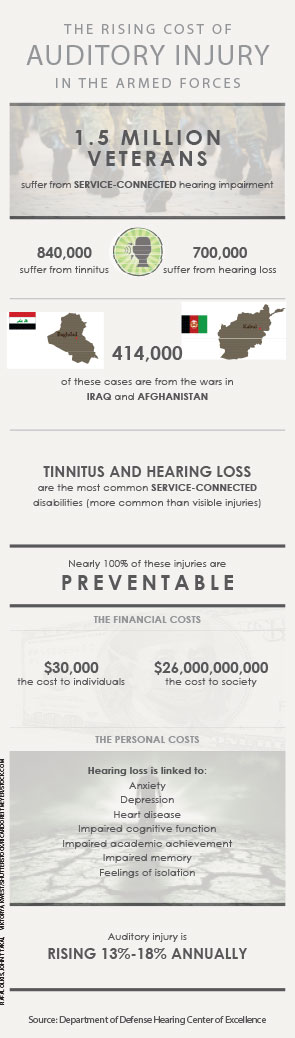
Unfortunately, Minnick is not alone. According to the Department of Defense Hearing Center of Excellence, 1.5 million veterans suffer from service-related auditory damage. Tinnitus and hearing loss are the most common service-related disabilities, consistently rated No. 1 and No. 2 on the Veterans Benefits Administration Annual Benefits Report distributed by the U.S. Department of Veterans Affairs. And, the number of service-connected hearing injuries seems to be increasing. According to the Hearing Center of Excellence, reports of auditory injuries are rising 13 to 18 percent annually.
Those injuries affect military readiness, because those who can’t hear well miss out on important environmental cues and warning signs, and military members and society experience its effects long after troops resume civilian life. “A lot of people who get out of the military are apt to go into a profession that requires communication skills, like a policeman or fireman,” said Kurt Yankaskas, program manager of the Office of Naval Research’s Noise-Induced Hearing Loss effort in Arlington, Va.
“Earning potential drops if you can’t communicate,” said Lt. Col. Mark Packer, MD, a neurotologist and director of the Department of Defense’s Hearing Center of Excellence. “So if you have a $30,000 drop in pay, that’s also $30,000 that’s not getting taxed. Hearing loss affects much more than just the individual and the individual’s family.”
Military physicians and safety officers are working in concert with civilian physicians, researchers and scientists to better protect troops’ hearing, and to restore hearing and quality of life post-service.
The Problem: Constant and Acute Noise Exposure
Military members experience unique auditory environments. While it’s not uncommon for civilians to work in chronically noisy environments, the duration and intensity of exposure is typically increased in military environments. “In the civilian sector, you have people working eight- to 10-hour days in fabrication, manufacturing and construction. Noise levels can be as high as 118 dBA,” Yankaskas said. “When you go to a military operation, the decibel level can be much higher, and it can be for 24 hours a day.”
Service members who work on ships or around airfields are chronically exposed to high levels of noise. But military members are also at risk for acute auditory insults. Active military operations in both Iraq and Afghanistan have increased the number of service members exposed to bombs, weapons fire and blasts, changing both the nature and mechanism of the auditory injury.
“Chronic noise exposure affects hearing within the sensory organ and cochlea; the hair cells are toxified by chronic exposure to loud noise,” Dr. Packer said. “Blast injuries can be much more traumatic. The peak pressures in the ear rise much more quickly, so the impact on the hearing system is not chronic and insidious but explosive. Some of the injuries we see from blasts not only show sensory hearing loss but also brain injury, tympanic perforation and disruption of the ossicular chain. The blast may also create flying debris, so there are secondary blunt impacts and trauma. And if you’re close enough, severe heat injuries and burns can also happen at the same time.”
Often, hearing is a secondary consideration; when a solider is injured, preference is always given to life-threatening injuries, and hearing injuries are often invisible. Some resolve quickly, for reasons physicians don’t quite understand. “Some patients who come in with complaints of hearing loss and tinnitus following an acoustic or blast-related injury will have subjective improvement fairly rapidly, but most patients do not. In the theater, audiometric testing is usually not available,” said Lt. Col. Mitchell Ramsey, MD, an otolaryngologist who served in Afghanistan. “Many factors contribute to presence or absence of recovery, including the blast intensity, innate inner ear tolerance to injury, co-existing conditions, prior trauma and probably many others, all of which need to be further researched.”
Field-related hearing injuries are often glossed over by active duty military personnel, who view their mission as more important than a non-life-threatening injury. Minnick said he “definitely noticed” his tinnitus and hearing loss in Iraq but didn’t seek medical treatment for his hearing issues until he left the service. “It’s not something you go to the doctor about,” he said. “It’s like, you’re alive and your ears are ringing. Big deal.”
—Lt. Col. Mark Packer, MD, Department of Defense’s Hearing Center of Excellence
The Challenge: Protecting Hearing Without Decreasing Awareness
The military has long championed hearing protection, but getting military members to use hearing protection consistently—especially in the field—is a constant challenge. “When you put anything in the ear, you change its sensitivity, and you change the ability to tell what direction something is coming from,” Yankaskas said.
Military safety officers stress the importance of hearing protection but also know that the ability to hear clearly enables troops to stay safe on the job. “You don’t want to decrease someone’s situational awareness and have them not know what’s going on around them,” said Lt. Amanda Fox, an aeromedical safety officer with the U.S. Marine Corps. “The flight deck of an aircraft carrier is a very high risk place to work; you take one wrong step, and you’re walking into the rotor blade of a helicopter or a prop arc of an airplane. You have to consistently know what’s going on around you; if you were to completely remove all audible warning signs, you couldn’t hear a jet sneaking up on you. You’re talking about a risk of death.”
Active service members, well aware of the risk of death, often value auditory awareness over hearing protection. “They tell you to wear hearing protection, but if you do, you really lose one of your senses,” Minnick said. “If you wear earplugs, you kind of take a chance of getting yourself killed because you can’t hear something as simple as the click of a grenade or the popping of a magazine. So, uniformly, I never wore earplugs, because I would rather have hearing loss than die.”
The Response: Better Hearing Protection, Improved Screening
That’s why the military is actively researching and developing better hearing protection. They’re also establishing widespread auditory screening programs, researching the genetics of susceptibility and investigating innovative treatments.
“We are working at creating hearing protection that is easier to use, is more comfortable to wear for really long periods of time and doesn’t deprive the soldier, sailor or airman of their need to communicate,” Yankaskas said. Most military members in high-noise areas now have access to custom-molded silicone earplugs. “The VA has really taken a proactive stand with technology such as active noise reduction [ANR] and custom ear molds,” Fox said. Silicone earplugs, created specifically for one military member, are designed to fit perfectly inside the external auditory. But even custom plugs can block essential outside noise and inhibit communication, so some military members, including pilots, now wear custom ear molds with radio communications embedded directly into the ear piece.
Meanwhile, the Navy’s Noise-Induced Hearing Loss program continues to investigate improved forms of hearing protection. “In one of our earlier projects, we were using a next generation low-power cochlear implant. In that came a signal processor, and the signal processor is smart enough so that it can differentiate gunfire from voice. It could shut down those bands for the proper length of time, so you don’t hear the gunfire, then enable normal conversation,” Yankaskas said. “We called it intelligent filtering. It’s tricky, though, because the brain does a lot of signal processing on its own, and putting that in a chip is a challenge.”
The Noise-Induced Hearing Loss Program and the DOD’s Hearing Center of Excellence are also investigating genetic susceptibility to hearing loss. “To date, we know that there are about 60 genes involved in hearing loss,” said Yankaskas. “We’re not sure how they all play together.” It is hoped that current animal studies will further advance the understanding of genetic susceptibility, allowing researchers and clinicians to better protect the hearing of vulnerable service members.“We are currently running some protocols to try to determine if there are people who ought to have different types of hearing protection or be taken out of certain sound environments before damage occurs,” Dr. Packer said. Even the possibility of genetic testing for susceptibility to hearing loss brings up a host of ethical issues. “It’s a bit of a sticky situation,” Dr. Packer said, “because you don’t want to necessarily discriminate on job opportunities. Some high-noise jobs have more pay or promotability attached to them.”
While the military continues to refine hearing protection, it also carefully tracks the hearing of those who serve. Currently, each branch of the service assesses an individual’s hearing as part of an overall military readiness program. “Just as individuals have to see a dentist and have their teeth assessed so we know that they’re not going to fall apart when the individual is deployed somewhere, troops have to have an audiogram that doesn’t show a significant loss or change so they can go to war and do their duties there,” Dr. Packer explained. “All of the services perform a periodic hearing assessment screen, depending on what line of work the individuals are in, and that’s a database called the Defense Occupational and Environmental Health Readiness System–Hearing Conservation. Anybody who is identified as working in a noise environment will have an initial audiogram … and then an annual audiogram to look for temporary or permanent shifts. They’re then triggered for further care and follow-up based on how they do in the program.”
Post-Service Care
Civilian otolaryngologists can help protect the hearing of military members by carefully assessing all veterans for hearing loss and tinnitus. According to the U.S. Department of Veterans Affairs, there are nearly 23 million veterans in the United States, and most experienced auditory insults during the course of their service. Knowing this, otolaryngologists should always ask patients who are veterans about their experiences in military service, said Dr. Ramsey. “Get a history, as best as possible, of what their noise exposure was and how many events and blasts and traumatic injuries they sustained.”
Use that information, as well as the data obtained by a baseline audiogram, to establish an individualized screening program. “Most people who have had accousting trauma in the form of chronic noise exposure or blast events should have their hearing monitored with serial audiograms,” Dr. Ramsey said. “They should be conducted yearly until the hearing levels are stable, but monitoring should continue long-term with audiograms every couple of years or as needed, depending on change in their symptoms.
Veterans may also experience typical age-related hearing loss at younger than usual ages. “There’s some evidence that acoustic trauma and injuries related to blast injuries may exacerbate age-related hearing loss,” Dr. Packer said. “So follow-up needs to be consistent, and rehabilitation strategies should be considered if the hearing decreases.”
Make sure veterans know that help is available; hearing loss and tinnitus aren’t just something they have to “live with.” Fred Minnick, the Iraqi war vet with hearing loss and tinnitus, was offered a hearing aid but declined. Helping service members become aware of the vast variety of hearing aids and assistance available, including barely visible and in-canal hearing aids, may increase acceptance of assistive devices that many young veterans still associate with old age.
Be aware that hearing loss or tinnitus in former military members may hint at other serious health conditions. “Anyone who has hearing loss, there’s a good chance that they have a psychological trauma deeply embedded in there too,” Minnick said. “Something I’ve noticed about doctors who have not worked with the veteran population before is that they tend to be very dismissive of their military service and just kind of treat the symptom. But for a lot of veterans, the war is still very much going on, and validation is huge for them. For many of us, there’s most certainly a connection between our hearing and the trauma we faced.”
—Lt. Amanda Fox, U.S. Marine Corps
Minnick advises otolaryngologists to familiarize themselves with the signs and symptoms of post-traumatic stress syndrome (PTSD), such as flashbacks, nightmares, numbness, hyperarousal and avoidance, and to make appropriate referrals as needed.
Because hearing injuries are frequently associated with brain injuries, balance problems and psychological issues such as PTSD, the Department of Defense is creating links between the Hearing Center of Excellence and other Centers of Excellence, including the Defense Centers of Excellence for Psychological Health and Traumatic Brain Injury. “We’re looking at ways to manage the patient holistically,” Dr. Packer said. “The impact of the injury on a patient’s life and function can be profound, and we want to help them.”
Leave a Reply