Comment: In this article, the authors shed light on a poorly understood otologic entity—idiopathic intracranial hypertension. Their thorough review of the causes, manifestations, and treatment options is essential reading for those encountering obese adults with headache. —Samuel H. Selesnick, MD
Explore This Issue
April 2018What is the role of the otolaryngologist in managing idiopathic intracranial hypertension (IIH) and related disorders?
Bottom Line: The knowledge base for idiopathic intracranial hypertension has greatly expanded over the past two decades. Otolaryngologists now play a key role in the co-management of this disorder including diagnosis, initiation of timely referrals, patient counseling, and treatment of related disorders. A keen understanding of this disorder and its management may optimize outcomes in a growing number of patients.
Background: IIH is defined as an elevation in cerebrospinal fluid (CSF) pressure with normal brain parenchyma, absence of ventriculomegaly, and no identifiable cause. This disease has been previously known under other names including pseudotumor cerebri syndrome, meningeal hydrops, and benign intracranial hypertension. Patients classically present with severe headaches, papilledema, and vision loss, which may progress to blindness in advanced or rapidly progressive cases. Due to the relative rarity of IIH, a number of significant controversies continue to surround its pathophysiology and management. Otolaryngologists play an increasingly important role in managing secondary and/or comorbid conditions. They may also be the first provider to suspect the diagnosis while treating related symptomatology. Given the dearth of studies focusing on this disease in the otolaryngic literature (only one published review over the past 20 years), otolaryngologists may feel ill-equipped to identify, diagnose, or assist in managing this disorder
Study design: Primary literature review, Centers for Disease Control and Prevention website, International Classification of Headache Disorders, Second Edition.
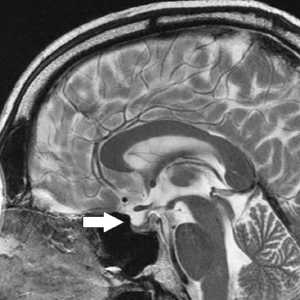
Midsagittal, T2-weighted MRI demonstrating compression of the pituitary gland (arrow) in a patient with idiopathic intracranial hypertension. This qualifies as a positive empty sella sign.

Axial, T2-weighted MRI demonstrating optic nerve sheath dilation (white arrow) and flattening of the posterior aspect of the right globe (asterisk)
© 2018 The American Laryngological, Rhinological and Otological Society, Inc.
Synopsis: A comprehensive review of the primary literature was performed from 1990 to 2016 utilizing keywords idiopathic intracranial hypertension, pseudotumor cerebri, benign intracranial hypertension, spontaneous cerebrospinal fluid leak, and encephalocele. The authors found that the incidence of idiopathic intracranial hypertension is increasing along with the obesity epidemic. Undiagnosed patients may present to otolaryngologists with pulsatile tinnitus, dizziness, sleep apnea, and spontaneous cerebrospinal fluid leaks. Although diagnosis is predicated upon imaging findings and lumbar puncture, radiographic signs including empty sella, optic nerve dilation, and globe flattening may suggest the diagnosis (Figures 1 and 2). The most effective intervention is weight loss combined with acetazolamide. Surgery is reserved for severe or refractory symptoms and can be highly morbid. Otolaryngologists are increasingly responsible for managing a number of secondary disorders including cerebrospinal fluid rhinorrhea and otorrhea. Failure to manage intracranial hypertension may lead to adverse surgical outcomes.
Citation: Stevens SM, Rizk HG, Golnik K, et al. Idiopathic intracranial hypertension: contemporary review and implications for the otolaryngologist. Laryngoscope. 2018;128:248–256.