But meeting the challenge is critical, particularly for otolaryngologists. Echoing Dr. Andersen, Dr. Kendall also highlighted the particular psychosocial needs of patients with head and neck cancer. “Head and neck cancer patients as a whole have significantly more psychosocial issues than other cancer sites,” he said. “So otolaryngologists as a group need to do this screening and have the resources available for follow-up more than other cancer sites.”
Explore This Issue
April 2016A number of resources are available to help integrate depression screening into routine cancer care. Among these are guidelines by the National Comprehensive Cancer Network (NCCN) and the American Society of Clinical Oncology (ASCO).
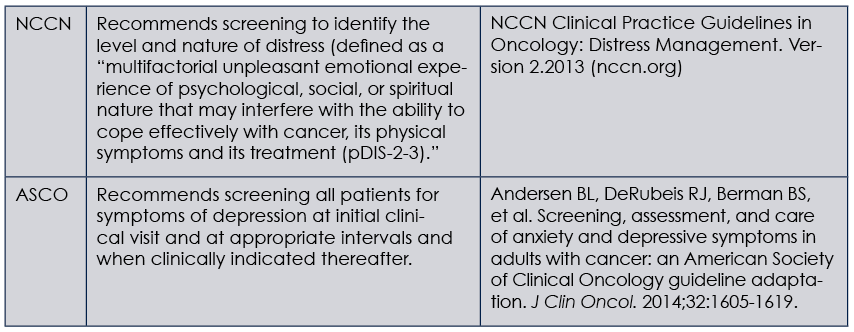
(click for larger image) Guides for Depression Screening in Cancer Patients
NCCN, National Comprehensive Cancer Network; ASCO, American Society of Clinical Oncology
Both of these guides offer algorithms on how to screen cancer patients for depression, as well as how to determine the next evaluation and treatment paths. A key determination that screeners need to make is which measure to use to screen for depression. Unlike the NCCN guidelines, which use a Distress Thermometer that covers a broad range of issues including but not limited to depression and anxiety, the ASCO guidelines recommend using tools designed and validated for depressive symptom assessment.
Dr. Andersen, who co-chaired the guideline panel, emphasized the recommendation to use the PHQ-9 measure as the most appropriate measure, as well as the Generalized Anxiety Disorder
seven-item (GAD-7) measure for anxiety symptoms. “These measures are validated and have been used successfully in many settings, including primary care,” she said. “Plus they correctly identify symptoms of anxiety and depression for which we have evidence-based treatment. The concept of distress is, unfortunately, vague and does not direct one to specific treatments.”
Dr. Shinn, who used the PHQ measure in her study, also recommended using this measure for depression screening, given its strong evidence base and psychometrics.
Dr. Kendall, who has previously used the NCCN Distress Thermometer to screen for distress in patients with cancer, said that the tool captures depression well. “If screening indicates that a patient is depressed, then referral for an assessment that can lead to an intervention is needed.” He stressed, however, the need to differentiate screening from assessment, saying that screening is only the first step and that the Distress Thermometer does a good job of screening. It is not an assessment tool, however; it only identifies patients for whom further assessment is recommended.