
© JPC-PROD / SHUTTERSTOCK.COM
One clinical decision that continues to present a challenge to many otolaryngologists is when to order a sleep study for a child in whom obstructive sleep apnea (OSA) or sleep-disordered breathing (SDB) is suspected and for whom an adenotonsillectomy (TA) is indicated.
Explore This Issue
September 2016Clinical guidelines published in 2011 by the American Academy of Otolaryngology–Head and Neck Surgery (AAO-HNS) have provided some guidance on this decision, as have guidelines published in 2012 by the American Academy of Pediatrics (AAP) and, to a lesser extent, those published in 2011 by the American Academy of Sleep Medicine (AASM).
Although all three guidelines contain similar suggestions, they differ significantly in their final recommendations, said Stacey L. Ishman, MD, MPH, surgical director of the Upper Airway Center at Cincinnati Children’s Hospital Medical Center in Ohio, in a recently published article (JAMA Otolaryngol Head Neck Surg. 2016;142:179-118).
In an interview with ENTtoday, Dr. Ishman emphasized that while the AAO-HNS guideline offers the most comprehensive guidance for otolaryngologists, the AAP guideline offers diagnostic options other than sleep studies and recognizes that sleep studies are not feasible in all situations.
Scott Brietzke, MD, MPH, an otolaryngologist at Walter Reed National Military Medical Center in Bethesda, Md., agreed that the AAO-HNS guideline is the most relevant for otolaryngologists and encouraged otolaryngologists to be aware of the other guidelines, while underscoring the need for clinical judgment in determining when and in whom to order a sleep study. “You can’t realistically perform a sleep study with every child who comes through your office door with a sleep complaint,” he said. “You have to balance the benefit of the study and a particular child’s situation.” Informed otolaryngologists, he added, generally use sleep studies judiciously, basing each decision on the patient’s individual situation rather than following a guideline blindly.
A Look at the Guidelines
The recommendations from the AAO-HNS guidelines on the use of polysomnography for SDB prior to TA in children are listed in “AAO-HNS Recommendations for When to Order a Sleep Study Prior to Adenotonsillectomy,” below.
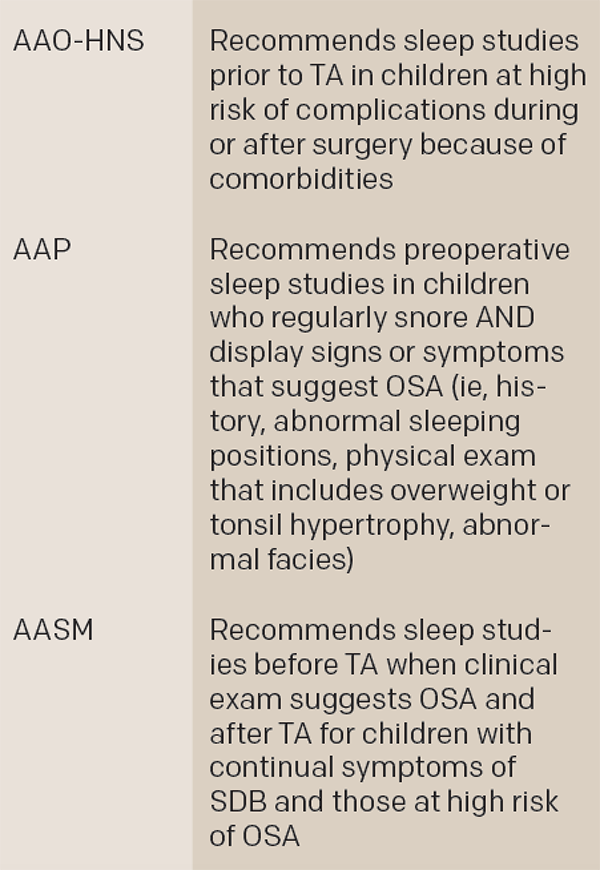
Key Differences among Three Guidelines
TA, adenotonsillectomy; OSA, obstructive sleep apnea; SDB, sleep-disordered breathing
Source: JAMA Otolaryngol Head Neck Surg. 2016;142:179-181
According to Dr. Ishman, the implication of the guideline is that a sleep study is always an option but is not required except in a subset of patients—namely, kids at increased risk for postoperative respiratory complications (see recommendation 1 on complex medical conditions, below).
Pell Ann Wardrop, MD, an otolaryngologist and medical director of the St. Joseph Sleep Wellness Center in Lexington, Ky., agreed. “Unless the child has risk factors such as obesity, craniofacial abnormalities, or neuromuscular disease, I feel a preoperative sleep study is optional,” she said. “I do the study when there is some question or doubt if a TA is needed.” She added that if only one sleep study is done, she recommends a postoperative sleep study. “It is vital to know when residual obstructive sleep apnea is present so the child can be appropriately treated,” she added. “Some of the treatment options, such as maxillary expansion, must be performed before the child matures.”
Dr. Brietzke described the thrust of the guideline this way: “If there is a lack of consistency within a physical exam and a history, you need a sleep study,” he said. “But if there is strong clinical evidence of sleep apnea, you can proceed with TA without a sleep study.”
Expanding on this statement, Dr. Breitzke highlighted the need for otolaryngologists to understand the difference between sensitivity and specificity of diagnostic tools when determining the value of a sleep study prior to TA. The clinical literature, he said, shows that the sensitivity of the clinical exam, combined with a history, is sufficient for establishing which child is a candidate for TA. “If a child comes in with large tonsils and has a convincing history of obstructive sleep apnea, it is reasonable to perform a tonsillectomy without a sleep study in many cases,” he said, adding that the statistics are “strongly on your side.”
He emphasized that the opposite is not true, however—ruling out sleep apnea is more difficult without a sleep study. “When you’re trying to exclude sleep apnea, or if the child has discordant tonsil size or if the history doesn’t fit, that is where a sleep study can be useful,” he said. He highlighted the importance of a sleep study after surgery in patients who remain symptomatic to obtain a clear diagnosis of sleep apnea prior to treatment with more surgery or continuous positive airway pressure (CPAP).
Tonsil Size
Both Drs. Ishman and Brietzke discussed the importance of tonsil size as a key component in the diagnostic assessment of whether or not to consider a sleep study.
Dr. Brietzke pointed out the difficulty of getting a clear estimate of tonsil size and the limited ability of old clinical scales for accurate measurement. He urged otolaryngologists to make a concerted effort to incorporate the use of three-dimensional measures from tools such as MRI or volumetric analyses of tonsils to get a more accurate estimate of tonsil size rather than just taking a quick look.
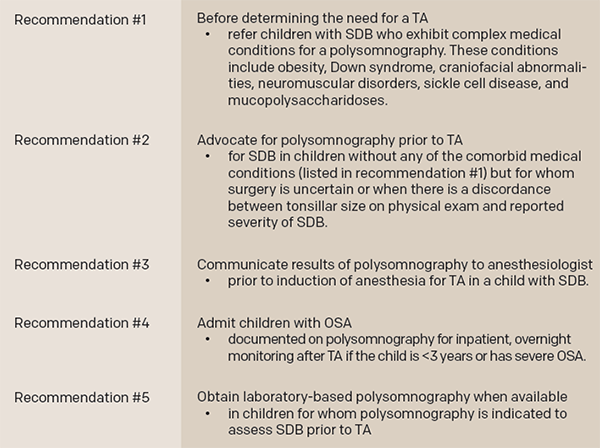
AAO-HNS Recommendations for When to Order a Sleep Study Prior to Adenotonsillectomy
TA, adenotonsillectomy; SDB, sleep-disordered breathing; OSA, obstructive sleep apnea
Source: AAO-HNS
For Dr. Ishman, children who present with few symptoms and very large tonsils fall into a group for which she often uses a sleep study prior to surgery to rule out unnecessary surgeries. “There are a group of kids who come in without many symptoms but with very large tonsils for whom surgery may not be necessary or the family may not be comfortable with surgery that is not absolutely necessary,” she said. “If you’re not sure that the symptoms and clinical exam match, I think sleep studies make a lot of sense.”
She emphasized, however, that most children with symptoms—and, particularly, daytime symptoms—and enlarged tonsils do not need a sleep study prior to surgery.
Other Considerations
Other children for whom Dr. Ishman says a sleep study prior to TA may be beneficial include those who are at high risk for postoperative complications if a sleep study will affect their management, such as changing their status from outpatient to inpatient or moving them from a floor bed to an intermediate care or ICU bed.
In addition, she emphasized that a sleep study is warranted for children with additional suspected sleep issues.
Feasibility
An important issue for otolaryngologists to consider when weighing the benefit of a sleep study is feasibility and accessibility for the patient. Highlighting the cost and time it takes to perform a sleep study, Dr. Ishman also emphasized the reality that a sleep study is not available to all patients.
She said the AAP guideline recognized this in its suggestion that clinicians consider other diagnostic options when a sleep study is not available. These include providing patients with a home oximetry study, video exam, or audio recording. “None of these is nearly as sensitive or specific as a full sleep study to diagnose sleep apnea,” she said, but she urged clinicians to try these options if a sleep study is desired but not available.
Mary Beth Nierengarten is a freelance medical writer based in Minnesota.
Key Points
- Three clinical guidelines have provided some guidance on when to order a sleep study prior to adenotonsillectomy in children, but the studies differ in their final recommendations.
- Otolaryngologists should understand the difference between sensitivity and specificity of diagnostic tools when determining the value of a sleep study prior to TA.
- Tonsil size is a key component of diagnostic assessment.
- Sleep studies are not always available to all patients.