Comment: Oncogene panels are costly tools that allow for risk-stratification of indeterminate thyroid nodules and theoretically may decrease the incidence of thyroid surgery for benign disease. The authors’ finding that the use of oncogene panels was in fact associated with higher rates of total thyroidectomy and central compartment neck dissection without an increasing yield of malignancy suggests that these costly tools may not have the intended effect on the management of indeterminate thyroid nodules. —Andres Bur, MD
Explore This Issue
September 2018What is the impact of oncogene panel results on the surgical management of indeterminate thyroid nodules (ITNs)?
Bottom line
OP evaluation was associated with higher rates of total thyroidectomy and central lymph node dissection without increasing the yield of malignancy or decreasing the rate of completion thyroidectomy.
Background: Several molecular marker tests are commercially available to characterize thyroid nodules with indeterminate cytology. Rule-out tests may avoid unnecessary diagnostic surgery, while rule-in tests may avoid the need for a completion thyroidectomy by identifying cancer before a diagnostic procedure. Total thyroidectomies may put patients at higher surgical risks to gain no clinical benefit.
Study design: Surgical management of 649 patients consecutively evaluated from October 2008 to April 2016 with a single nodule biopsied and indeterminate cytology.
Setting: Lee Moffitt Cancer Center and Research Institute, Tampa, Florida.
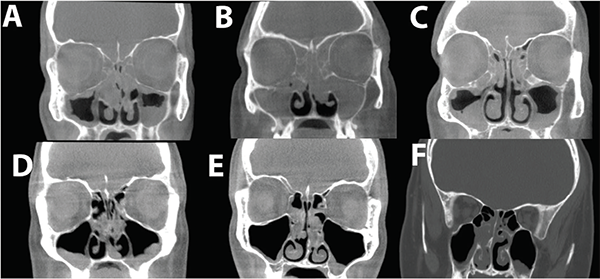
Radiological characteristic of eCRS and CCAD. Representative CT scan images of eCRS, with complete opacification of ethmoids and diffuse mucosal involvement of the maxillary sinuses (A–C). This is in contrast to CCAD where there is a central focus of the mucosal disease due to middle turbinate polyposis. If the sinuses are involved, the roof or lateral wall tends to be relatively normal (D–F).
Credit: © 2018 The American Laryngological, Rhinological and Otological Society, Inc.
Synopsis: Comparisons were done between the oncogene panel (OP) and control groups, and between OP_positive and OP_negative. Of the 938 original patients, 649 had just one thyroid nodule biopsied and were included for the analysis. Resection rate and cancer prevalence were not significantly different between control and OP groups, but the odds of having a total thyroidectomy for the OP group over the control group were 2.6, and 12.1 for OP_positive over OP_negative. OP evaluation increased the odds of being treated with total thyroidectomy by 160%. The odds ratio for central lymph node dissection was 1.7 in the OP group over the control group, and 5.7 in OP_positive over OP_negative. Malignancy prevalence was higher in OP_positive than in the OP_negative nodules treated with total thyroidectomy or central lymph node dissection. Overall, malignancy prevalence was 26%, and was significantly higher in OP_positive compared with OP_negative. Most malignancies (64%) were low-risk; 33% were intermediate risk and 3% were high risk. Limitations include patients coming from a single center and the analysis of different OPs.