Is serial in-office laser treatment for vocal fold (VF) leukoplakia effective for long-term disease control with minimal morbidity?
Bottom line
Serial outpatient potassium titanyl phosphate (KTP) or pulsed dye laser (PDL) treatment of VF leukoplakia is effective for disease control with minimal morbidity and preservation of voice quality.
Explore This Issue
July 2017Background: Leukoplakia is a clinical diagnosis indicating the presence of keratin on the VF epithelial surface. This diagnosis portends a risk of malignant transformation, with the severity of dysplasia associated with an increased rate of malignant degeneration. The management of leukoplakia poses a clinical dilemma because leukoplakia carries with it a risk of malignant transformation regardless of dysplasia grade, and it often recurs after treatment. There is no consensus on treatment, with surgeons offering varying degrees and frequency of surveillance, differing thresholds for repeat biopsy, and options of repetitive ablative or excisional management. Recently, treatment with in-office laser has become a common strategy. Although there are studies demonstrating the efficacy of in-office laser treatment of VF leukoplakia, these works are often based on a small series that may not be specific to leukoplakia, do not employ serial treatment, have short-term follow-up, and do not use objective methods to quantify disease regression (See Figure 2).
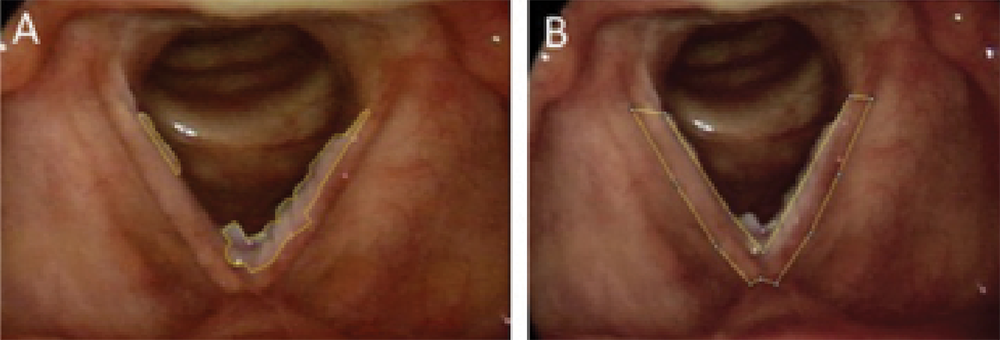
Figure 2. Determination of % lesion regression. (A) Average lesion area (three measurements) = 1,831 pixels. (B) Average full VF area (three measurements) = 6,924 pixels. Percent VF covered by the lesion was determined by (A/B) × 100% = (1,831/6,924) × 100% = 26.4% of the VF covered by lesion. This % was then compared with the postoperative picture % to determine regression.
Credit: Copyright 2017 The American Laryngological, Rhinological and Otological Society, Inc.
Study design: Retrospective review (2008–2015).
Setting: New York Eye and Ear Infirmary of Mount Sinai.
Synopsis: Forty-six patients with VF leukoplakia treated by in-office KTP or PDL were included. Median follow-up from final laser treatment was 19.6 months. Main outcomes included: 1) rate of disease control, 2) percentage of disease regression using ImageJ analysis. Secondary outcomes included vocal assessment using the Voice Handicap Index-10 (VHI-10). Patients underwent a median of two (range: 1–6) in-office laser treatments. Time between treatments was median 7.6 months. After final treatment, 19 patients (41.3%) had no disease; two patients (4.3%) progressed to invasive cancer; overall disease regression was median 77.1%; and VHI-10 score decreased by median 5. Thirty-one patients (67.4%) were responders (controlled with in-office treatment only); 13 patients (28.3%) who required operative intervention and two patients (4%) who underwent radiation were categorized as failures. Compared with responders, failures demonstrated significantly shorter duration between treatments (median 2.3 vs. 8.9 months) and significantly less regression (median 49.3% vs. 100%).