Improving Inpatient Resident Hand-Offs and Transitions of Care
 To explore ways to improve the accuracy of resident handoffs, a team from Virginia Commonwealth University in Richmond undertook a quality improvement (QI) initiative. Their work was presented by Austin N. DeHart, MD, who is now a fellow in pediatric otolaryngology at Arkansas Children’s Hospital in Little Rock.
To explore ways to improve the accuracy of resident handoffs, a team from Virginia Commonwealth University in Richmond undertook a quality improvement (QI) initiative. Their work was presented by Austin N. DeHart, MD, who is now a fellow in pediatric otolaryngology at Arkansas Children’s Hospital in Little Rock.
Explore This Issue
July 2019“We know that 20% to 40% of malpractice claims are associated with patient handoffs, communication failures, and transitions of care,” said Dr. DeHart. “The ACGME has new requirements that programs ensure and monitor effective and structured handoffs in order to facilitate the continuity of care and patient safety.”
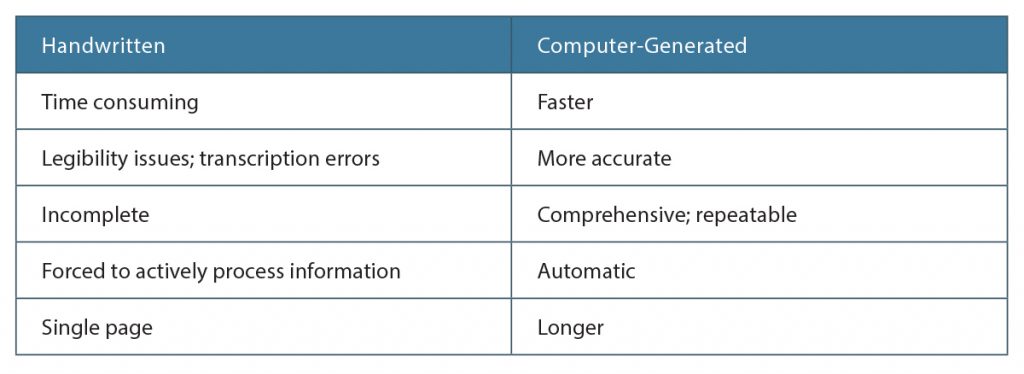
Their institute is a tertiary care academic hospital with residents who rotate among multiple teams and cross-cover call, so there are numerous handoffs every day. “We were using a handwritten list to keep track of patients during rounds and handoffs, which took a lot of time to make and were variable in quality,” she said.
She and her team wanted to see if a computer could improve the process and initiated a QI project to determine if they could create a computer-generated list that would save time and improve accuracy. They performed a retrospective analysis of the handwritten lists over a one-month period and found large variability in the accuracy and reliability among the lists, depending on who made them. They used this information to obtain support from the bioinformatics department to contract with a third party to create a computer-generated list.
“Once the residents were familiar with the computer-generated list, we held a workshop where all team members created both lists and compared the processes,” she said. A survey of the trainees revealed that 100% found the computer-
generated lists helpful and 80% indicated that the computer-generated lists were better for patient care; 70% preferred the computer-generated list to the handwritten list.
“One of the positive aspects of a handwritten list is that it forces you to actively think about what is required,” said Dr. DeHart. “But, obviously, too many things are being missed with this method.”
Elizabeth Hofheinz is a freelance medical writer based in Louisiana.
Mentorship Program Goals
- Early exposure to the profession of otolaryngology
- Early introduction of surgical mentorship
- Feedback-oriented longitudinal clinical experience
- Education on the residency application process
- Career advice, networking, and research opportunities
- Focus on professionalism.